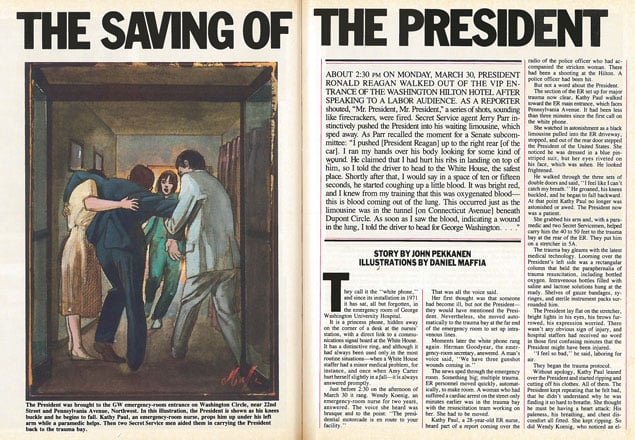
About 2:30 PM on Monday, March 30, President Ronald Reagan walked out of the VIP entrance of the Washington Hilton Hotel after speaking to a labor audience. As a reporter shouted, “Mr. President, Mr. President,” a series of shots, sounding like firecrackers, were fired. Secret Service agent Jerry Parr instinctively pushed the President into his waiting limousine, which sped away. As Parr recalled the moment for a Senate subcommittee:
“I pushed [President Reagan] up to the right rear [of the car]. I ran my hands over his body looking for some kind of wound. He claimed that I had hurt his ribs in landing on top of hlm, so I told the driver to head to the White House, the safest place. Shortly after that, I would say in a space of ten or fifteen seconds, he started coughing up a little blood. It was bright red, and I knew from my training that this was oxygenated blood—this is blood coming out of the lung. This occurred just as the limousine was in the tunnel [on Connecticut Avenue] beneath Dupont Circle. As soon as I saw the blood, indicating a wound in the lung, I told the driver to head fur George Washington. . . .”
They call it the “white phone,” and since its installation in 1971 it has sat, all but forgotten, in the emergency room of George Washington University Hospital.
It is a princess phone, hidden away on the corner of a desk at the nurses’ station, with a direct link to a communications signal board at the White House. It has a distinctive ring, and although it had always been used only in the most routine situations—when a White House staffer had a minor medical problem, for instance, and once when Amy Carter hurt herself slightly in a fall—it’s always answered promptly.
Just before 2:30 on the afternoon of March 30 it rang. Wendy Koenig, an emergency-room nurse for two years, answered. The voice she heard was brusque and to the point: “The presidential motorcade is en route to your facility.”
That was all the voice said.
Her first thought was that someone had become ill, but not the President—they would have mentioned the President. Nevertheless, she moved automatically to the trauma bay at the far end of the emergency room to set up intravenous lines.
Moments later the white phone rang again. Herman Goodyear, the emergency-room secretary, answered. A man’s voice said, “We have three gunshot wounds coming in.”
The news sped through the emergency room. Something big; multiple trauma. ER personnel moved quickly, automatically, to make room. A woman who had suffered a cardiac arrest on the street only minutes earlier was in the trauma bay with the resuscitation team working on her. She had to be moved.
Kathy Paul, a 28-year-old ER nurse, heard part of a report coming over the radio of the police officer who had accompanied the stricken woman. There had been a shooting at the Hilton. A police officer had been hit.
But not a word about the President.
The section of the ER set up for major trauma now clear, Kathy Paul walked toward the ER main entrance, which faces Pennsylvania Avenue. It had been less than three minutes since the first call on the white phone.
She watched in astonishment as a black limousine pulled into the ER driveway, stopped, and out of the rear door stepped the President of the United States. She noticed he was dressed in a blue pinstriped suit, but her eyes riveted on his face, which was ashen. He looked frightened.
He walked through the three sets of double doors and said, “I feel like I can’t catch my breath .” He groaned, his knees buckled, and he began to fall backward. At that point Kathy Paul no longer was astonished or awed. The President now was a patient.
She grabbed his arm and, with a paramedic and two Secret Servicemen, helped carry him the 40 to 50 feet to the trauma bay at the rear of the ER. They put him on a stretcher in SA.
The trauma bay gleams with the latest medical technology. Looming over the President’s left side was a rectangular column that held the paraphernalia of trauma resuscitation, including bottled oxygen. Intravenous bottles filled with saline and lactose solutions hung at the ready . Shelves of gauze bandages, syringes, and sterile instrument packs surrounded him.
The President lay flat on the stretcher, bright lights in his eyes, his brows furrowed, his expression worried. There wasn’t any obvious sign of injury, and hospital staffers had received no word in those first confusing minutes that the President might have been injured.
“I feel so bad,” he said, laboring for air.
They began the trauma protocol.
Without apology, Kathy Paul leaned over the President and started ripping and cutting off his clothes. All of them. The President kept repeating that he felt bad, that he didn’t understand why he was finding it so hard to breathe. She thought he must be having a heart attack: His paleness, his breathing, and chest discomfort all fitted. She kept ripping. So did Wendy Koenig , who noticed an elegant RR monogram on his shirt just before she tore it off.
Now standing at the bottom end of the President’s stretcher was the tall, quiet figure of Dr. Daniel Ruge, his personal physician. Ruge had been at the Hilton. After making certain none of the injured on the sidewalk was the President, he had jumped into an official car that followed the presidential limousine to GW. A well-known and respected neurosurgeon, he now put his hand on the President’s foot to monitor his pulse, which was steady and strong. Ruge offered several reassuring words to the President.
A crowd of Secret Servicemen, DC policemen, and hospital personnel hovered in the ER. Radios squawked. The sounds of sirens still echoed in the streets outside. The noise in the ER mounted. At times it was nearly deafening.
Wendy Koenig put the blood-pressure cuff on the President’s arm. She pumped it up and waited for the thumping sound of the pulse in her stethoscope.
Not a sound.
“I can’t hear anything,” she yelled. “I can’t get a systolic pressure.”
The President is arresting, she thought, right here in front of me. She had to fight back tears. She remembered a nightmare she’d had a few months earlier, just after Ronald Reagan was elected President. He had been in the ER, ill and under her care. The memory of the nightmare was vivid. And now it was happening.
She pumped up the cuff again. Nothing.
She couldn’t tell whether the President’s blood pressure was too low or the noise level in the ER too high.
She pumped up the cuff one more time, and now she palpated an artery with her fingers. She felt the first throb, somewhere between 50 and 60 systolic, an ominously low pressure, suggesting shock. Normal would be 130. The President was at this moment more dangerously ill than the public would ever realize.
Less than two minutes had elapsed since Ronald Reagan had walked in.
• • •
Cindy Hines, a medical technician, had immediately and automatically begun inserting large-bore intravenous (IV) lines into the arm of the man lying in front of her. In the excitement she’d never learned who he was. Not until she had put an IV line in his arm did she take the time to look up and see his face.
In trauma resuscitation there is nothing more precious than time; speed is the inviolable first principle. It is during the “golden hour”—the first 60 minutes—that most trauma patients are either saved or lost. Most of those lost die from shock, caused when the body’s blood volume becomes so depleted that there is not enough to go around. Even people in deep shock can be resuscitated. But if too much time is lost before shock is reversed, the major organs can’t support the body, and the patient dies. He or she may not die that minute or even that day, but death is inevitable.
The President was ashen because his involuntary nervous system had taken over, redirecting his blood flow away from his skin and extremities and into his vital organs, which had a far more urgent need for it. There is little question that in those first few minutes he was very close to shock if not in shock itself- as one of his physicians later remarked, the President was “on the brink.”
No one knew what was wrong, because there was no obvious sign of injury. Jerry Parr, the Secret Serviceman who had landed on the President in the limousine and then directed it to GW after he spotted blood on the President’s mouth, an act which probably saved Ronald Reagan’s life, thought he might have cracked one of the President’s ribs. But in those first two or three minutes none of the nurses noticed any blood or other possible sign of injury. It was only when Kathy Paul saw blood on the President’s hand and Cindy Hines noticed blood inside his mouth that they knew he wasn’t arresting; he was hurt.
Urgent messages had already been dispatched by the paging operators throughout the hospital: “Trauma team to the emergency room.” Many doctors were also paged individually.
A meeting of department chairmen and administrators on the top floor of the Bums Building, just across 23rd Street from the main hospital, was interrupted when Michael Barch, administrator of the Medical Center, answered his page. He came back in the room and announced that the meeeting was over because the President of the US was across the street in the emergency room.
Three physicians—surgical residents David Gens, Brad Bennett, and Paul Colombani—meeting for their regular Monday-afternoon discussion group in the third-floor on-call room heard their pagers go off at the same time. Odd. Bennett answered. “You’re wanted in the emergency room. Stat.”
Stat, says a doctor, “means you get there before your clothes.”
They came running.
Dr. Sol Edelstein, director of the emergency room, had just driven his wife home from the hospital, where she’d given birth to a son five days earlier. She had extracted a promise from him that he would take a week off. His pager went off minutes after they walked in the door.
Edelstein made the 20-minute drive from his home in Glen Echo Heights to the hospital in seven minute’ flat.
“I can’t breathe,” the President repeated. The nurses took turns holding his hand and reassured him. He lay with his arms at his sides, his expression worried, but he was conscious and· calm.
Three IV lines were now pushing fluids and blood into him, boosting his blood volume.
Perhaps three minutes—at most—had elapsed since the President’s arrival.
• • •
Dr. Wesley Price, a senior resident who was not on the trauma team but who hurried down from an upstairs pathology office when he saw the motorcade heading for the hospital, and Dr. William O’Neill, an intern on the trauma team, were the first GW physicians to treat the President.
O’Neill thought his page was routine until he rounded the final corridor to the ER. From there he noticed a black limousine parked where the ambulances usually were and he saw the presidential seal. “I hope it’s not the President,” he thought to himself as he headed into the emergency room.
Secret Servicemen made quick checks and allowed Price and O’Neill to pass to the trauma bay. Both were stunned when they saw the President lying on the stretcher with lines going into his arms.
“Can anybody tell me what happened?” Price asked. No one seemed to know.
They made a rapid assessment. O’Neill, who had worked in the emergency room as an undergraduate, had seen a lot of trauma. “You develop an immediate gut feeling as to who is really sick and who isn’t,” he said later. When he saw the President he felt he was looking at someone potentially in jeopardy—on the brink.
The President’s palpable blood pressure was up to 78 systolic—still abnormally low but an improvement. The fluids were doing their job. The President’s pulse was 88 and steady, another encouraging sign.
“Mr. President, where do you hurt?” O’Neill asked.
“My chest hurts and I’m having trouble breathing.”
“Do you know what happened?”
“Not really.”
“Are you hurting anywhere else?”
“No, I don’t think so.”
No other symptoms were evident. The President was thinking clearly and able to move all four limbs. To ease his breathing, they propped his head up about 20 or 30 degrees.
Wesley Price, the son of a North Carolina preacher, put a stethoscope to the President’s chest and listened for breath sounds. Listening to the right lung, he heard crackling noises. The breath sounds on the left side were markedly diminished. Air was not moving in and out freely. As Price continued to listen to the left side he noticed a small, jagged slit, like a buttonhole, but more vertical than horizontal, just below the President’s armpit. There was a black spot around it and blood was trickling out.
More doctors were arriving.
Dr. Drew Scheele, a general-surgery intern who had been a helicopter pilot in Vietnam, where he’d seen many gunshot wounds, including his own, looked at it with Price. They both realized they were looking at the entry wound of a bullet. Two other new arrivals, Gens and Bennett, also thought it was an entry wound. Price turned to Jerry Parr, the Secret Serviceman who had thought he’d broken the President’s rib . “It looks like he’s been shot,” Price said.
Dr. Ruge gave Ronald Reagan this news. The President nodded. Ruge added reassuringly: “Everything is okay.”
Wendy Koenig asked the President if he’d had a tetanus shot recently. He couldn’t remember. She gave him one.
They gently rolled the President from side to side, looking for an exit wound. There was none, so the bullet had to be in the chest or abdomen. Then Price and O’Neill thought they noticed distended neck veins, a disturbing sign because it could be caused by cardiac tamponade, the filling of the pericardia! sac surrounding the heart. This could mean the bullet had actually struck the heart. On the other hand, heart sounds were normal. It was too early for certainties.
The physicians treating the President during these first few critical minutes were all very young. Most were around 30 and had been doctors for only the three or four years of their residency training. Bill O’Neill, an intern, had been a doctor for only eight months.
They wondered what was going on in his mind when they poked at him, listened to him, and tried to speak reassuringly to him. He knew none of them; Dr. Ruge was the only person familiar to him. They realized the President was worried, perhaps even frightened, although he was masking it well. They admired his coolness.
The young physicians had moments when, for a flashing second or two, they were awed by the enormity of what they were doing. And more than once the thought skittered across the mind: My God, this is the President—I’d better not screw up. For some, it caused a temporary reluctance to treat him.
But most of them had completed a three-month rotation at the shock-trauma unit in Baltimore, the premier trauma unit in the country. They also had gained considerable experience with trauma at GW. Moreover, the trauma team—formed at GW just three years earlier—had, under the direction of Dr. Joseph Giordano, drilled and drilled until they knew the treatment protocol instinctively.
Now the protocol was doing precisely what it was designed to do. For in times of serious injury, or confusion, or exhaustion, or all of these, the protocol becomes the thinking process—it tells the team what to do and how to do it. It is based on logic and is designed for speed. Critical to its success is aggressive overtreatment, searching everywhere so that not only the most obvious injuries are treated, but also the smaller, more insidious ones that can quietly kill the patient.
Following protocol, David Gens examined the President’s abdomen. He found no tightness, no sign of abdominal injury.
The President’s left chest was thumped with hands and fingers. Where it should have sounded hollow, there was a dull, flat resonance. His left pleural cavity was filling with blood.
Dr. George Morales, an anesthesiologist, now placed an oxygen mask over the President’s nose and mouth and kept reassuring him that everything was under control. The President repeated that he was having difficulty breathing. Someone had delicately placed a sheet over the President’s lower body after Dr. Gregory Hornig, an intern, had inserted a Foley catheter into his bladder to monitor urinary function.
Less than twelve minutes had passed since President Reagan’s arrival at GW.
• • •
Press secretary James Brady, 40, grievously wounded, was wheeled into trauma bay 58, right next to the President, separated only by a curtain. His arrival was quickly followed by that of Secret Serviceman Timothy McCarthy, 31, the least seriously wounded victim of the Hilton shooting. He was put in ER 3, just a few feet from the trauma bay. Some doctors and nurses split off to attend Brady and McCarthy.
The crowd in the ER kept growing; the noise increased; the air grew hot. Brad Bennett, a member of the trauma team, tried to remove everyone without a specific function from the President’s trauma bay. When he wasn’t doing that he was squeezing the red-cell blood packs to force the vital, oxygen-carrying cells into the President as fast as possible. Farther away, Doctors Dennis O’Leary and Sol Edelstein and administrator Mike Barch were also attempting to control the crowd. Excitement, tension, and fear gripped many in the ER, but panic was never a factor.
Senior faculty physicians continued to arrive, some still perplexed about why they had been summoned. One asked aloud: “Why the hell was I paged?” A curtain of people in front of him parted slightly and he saw the face of the President. He said no more.
The attending physicians asked Dr. Ruge, who was observing but not intruding, about the President’s health.
Blood type?
0 positive.
Any allergies?
Adhesive tape and sulfa drugs.
Any medical conditions?
An old prostatectomy, fifteen years ago. Nothing else.
The President’s blood pressure continued to rise steadily.
A chest tube was readied to remove the blood flooding his left lung. Wesley Price put a shot of Xylocaine into the President’s side, between two ribs, to dull the pain of the incision and tube insertion. As he prepared to cut, he heard the voice of Dr. Joseph Giordano, a faculty surgeon and head of the trauma team.
“You’d better let me do this one,” Giordano said. Price realized it was appropriate that the senior physician take over.
Giordano cut an opening through the skin and muscle wall. He stuck his finger into the opening to make certain he was into the pleura, put a clamp on the tube, and popped it into the hole. The President winced at the pain. The other end of the tube was connected to a suction device called a Pleur-evac. Wendy Koenig had to fill the Pleur-evac partially with sterile water to begin the suction process. In the excitement, she poured a bottle of water into her shoe. The next time she hit the target.
Blood gushed out of the President’s chest tube—I ,300 cc’s of it, perhaps a fourth of his total supply. No one was alarmed; chest tubes normally pull out a lot of blood when they are first inserted into a wounded chest.
But the blood continued to come, and one man was keeping an especially wary eye on it.
Dr. Benjamin Aaron had been in his office in the Bums Building doing paperwork when he was abruptly paged to the ER. He had been up until 2 AM the night before, repairing a complication from a previous open-heart operation, and earlier that day he’d done a coronary bypass operation.
A 48-year-old thoracic (chest) and cardiac (heart) surgeon, and a Navy surgeon for 22 years before he came to GW in 1979, Aaron is calm and understated, a man not only accustomed to the tight tolerances and demanding pressures of cardiac surgery but one who thrives on them. Shortly after he arrived at the ER, he realized that the President was not in mortal danger. An arterial line had been hooked to the President’s left wrist, and doctors were getting continuous readouts of his blood pressure and pulse on a display monitor. His blood pressure was now above 100. His pulse was steady. Aaron saw that the EKG monitor reading indicated a strong, normal heartbeat.
Usually, when a chest tube is inserted and the lung re-expands, the injured vessels close off and the bleeding stops. In about 90 percent of all cases involving this type of chest wound, surgery is not performed.
But in Ronald Reagan’s case the bleeding didn’t stop. That was the first thing that disturbed Ben Aaron. The second was the color of the blood. It was not the bright red of freshly oxygenated blood. It had a darker, ruby cast to it, suggesting venous blood. Aaron had opened thousands of chests in his day and he knew that venous blood coming out of the chest meant some part of the pulmonary artery—through which venous blood is pumped from the heart to the lungs—was injured.
He tried to drive from his mind the thought that he was treating the President of the US, tried to concentrate on the simple thought that he was attending a 70-year-old man with a gunshot wound. He said little. He listened to the President’s lungs. He watched the ruby-colored blood flowing out of the President’s chest.
• • •
In 58 there was little hope for James Brady. His injury was hideous. The hole through his skull, just above his left eye, leaked cerebral tissue freely. His eyes were so swollen that they could no longer be examined to see if his pupils were fixed and dilated, and the only hopeful sign was that on arrival they still reacted to light. His left eye had swollen to the size of an egg. He was unconscious, but his body sometimes thrashed.
The bullet had traversed the two hemispheres of his brain, and nearly 90 percent of such wounds are fatal. Because of the injury, his brain had begun to swell. When swelling is uncontrolled, the brain “herniates” down—the only direction it can go in the confines of the skull—and there it compresses the brain stem, which regulates heartbeat and other vital functions of the body. When this happens, the patient dies.
The swelling had already caused an enormous increase in Brady’s intracranial pressure—which in turn shot his blood pressure up to 240/160, a very high reading. It was his body’s way of compensating, of trying to force blood into the brain to oxygenate the tissues. But he had used up all his reserves. Moreover, blood pressure that high can cause other serious problems.
Everything that could be done in those first few minutes was done, and speedily. Major credit for this should go to Dr. Judith A. Johnson, an anesthesiology resident who switched from treating the President, when she realized that there were enough people to attend to him, to Brady.
She put an endotracheal tube into Brady’s windpipe, a delicate procedure when a patient has a head wound as serious as Brady’s. To prepare him for it she had given him Pentothal and a curare- type drug to paralyze him so he would not fight the tube he needed for breathing. His head was elevated 45 degrees to relieve intracranial pressure.
Working with Dr. Jeff Jacobson, a neurosurgery resident, Dr. Johnson gave Brady a large dose of mannitol and steroids to decrease the intracranial pressure.
All this was done within Brady’s first eight to ten minutes in the ER.
Dr. Arthur Kobrine, a young, acerbic, and highly skilled neurosurgeon on the GW faculty, was paged to the trauma bay, where he saw Dr. Ruge, a former teacher and friend of his at Northwestern Medical School. Ruge once taught there and Kobrine did part of his residency there, and they had become close friends. Ruge had asked Kobrine if he would examine Brady. Kobrine was blunt with Dr. Ruge after the examination.
“Dan,” he said, “I don’t think he’s going to make it, but I think we ought to operate.”
Ruge told him to do whatever he thought he had to do.
It was crucial that Kobrine move quickly, and he did. Within 20 minutes of Brady’s arrival at the hospital he was wheeled into the CT scan room. There, thanks to a computerized X-ray technique called tomography, doctors would see the precise extent and location of his injuries and would know if surgery held out any hope for what seemed to be a doomed patient. Despite the medication he was receiving, Brady’s brain was continuing to swell.
• • •
In ER 3, Secret Serviceman Tim McCarthy was in stable condition. The only outward sign of injury was a small, bloodless hole in his right chest. A peritoneal lavage was performed- a procedure in which sterile fluid is put into the abdominal cavity and washed out to determine if any blood is present. There was. Exploratory surgery would be necessary.
McCarthy was apprehensive but remained calm. He asked about the President. Dr. Stephen Pett, a thoracic surgeon, and Doctors Jack Fisher and Norman Odyniec were among those attending him.
It was several days later that McCarthy talked about his ordeal. As he lay on the sidewalk at the Hilton, he said, he could feel no wound, no blood, although he thought he’d been hit twice. Then a paramedic rushed up to him and asked if he’d been hit. I think so, McCarthy said. The paramedic couldn’t find a wound, and told McCarthy he didn’t think he’d been hit. Well , then, you’d better shoot me, McCarthy thought to himself, I don’t want the world to think I just fell down out here.
• • •
Perhaps eighteen minutes had passed since the President’s arrival at the hospital. Ben Aaron kept watching the rubycolored blood flow out of the President. Not a flood, but more than a trickle.
The President’s blood pressure was now nearly normal. His color was better, but he still couldn’t breathe without difficulty. If the President kept losing blood, the doctors would not be able to keep giving him fluids indefmitely. When blood is replaced by fluids , the patient’s hemoglobin diminishes; even though the blood pressure is normal, the tissues are deprived of oxygen, and the kidney, heart, and lungs lose function. If whole blood is administered for too long, the patient’s blood loses its ability to clot. That possibility was approaching.
A portable X-ray machine was wheeled into the trauma bay , and within two minutes a chest film was taken and developed. Dr. David Rockoff, the head of chest radiology, was there to read it.
It showed that, with the blood draining out through the chest tube, the lung had re-expanded. Rockoff also noticed an irregularly shaped, hazy area where blood remained in the left chest cavity. Then he saw a small, slender metal fragment shaped almost like a comma in the shadow of the heart. It was the bullet. Ben Aaron also looked at the film. According to their viewing angle, the bullet could have hit the heart, the aorta, or the pulmonary artery. But the dark color of the blood coming from the President’s chest still suggested that its source was the pulmonary artery, not the aorta, which produces bright-red blood.
Rockoff, a highly respected member of the GW faculty, needed to know the caliber of the bullet. If it was a .22, they were seeing all of it. If it was a larger caliber, another fragment might have hit a rib and been deflected into the abdominal cavity.
He turned to a Secret Serviceman standing next to him and asked: “What caliber bullet was it?”
The Secret Serviceman said he didn’t know but would find out. What followed was one of the most inexplicable incidents in the President’s shooting.
Rockoff listened as the Secret Serviceman turned to a superior and said, “They’ve got to know the caliber.”
The agent’s superior said, “Then call the FBI. They’ve got the gun.”
The Secret Service agent went to a nearby phone and called the FBI. This is what was then overheard in the GW emergency room:
“What do you mean you ‘can’t’ tell me?” the Secret Serviceman said. “The doctors here have to know.”
He turned to his superior and shouted: “They won’t tell me.”
“You tell them they’ve got to tell you! It’s the President.”
His voice rising, the Secret Serviceman told the FBI: “We’ve got to know, and we’ve got to know now!”
There was a moment’s silence before the Secret Serviceman turned to Rockoff and said: “It’s a .38.”
Rockoff, stunned by this information, relayed it to colleagues. “It’s a .38,” he said. “We need a belly film to look for the rest of the bullet.”
This occurred approximately 20 to 25 minutes after the President was admitted to the ER. The error was never corrected by any of the authorities, nor was the reason for it ever given. Although much of the nation was soon to learn from television that a .22 caliber had been used, the physicians treating the President were not watching television. They worked now under the assumption that he had been shot with a .38 and they would continue to assume that until, approximately 60 to 90 minutes later, an intact .22-caliber bullet was removed from Tim McCarthy, confirming that a .22 caliber was the weapon.
An abdominal X-ray—the “belly film”—of the President was taken immediately. One would have been taken anyway, but if the doctors had had correct information about the caliber of the bullet, it would have been done later. If time had been a more critical factor, the misinformation about the bullet could have been costly.
The abdominal film was negative. The doctors then assumed—because they could find no evidence of a bullet anywhere else—that it had probably hit something and shattered, and only a fragment had entered the President.
Dr. Neofytos (Newt) Tsangaris, acting chairman of surgery, was on the phone. “We’re probably going to need three ORs,” he said. Only two operating rooms were available now; another would be ready in a few minutes.
Nancy Reagan was ushered through the crowd in the ER and into the trauma bay. She held her husband’s hand and leaned over to kiss his forehead. “Honey, I forgot to duck, he said.”
His wife was controlled, but her face registered worry and fear. After a brief visit, she returned to the small interview room at the entrance to the ER to join Edwin Meese, James Baker, and Lyn Nofziger, members of the President’s staff.
Gens and Bennett tried to insert a large bore line into the President’s jugular vein to push in more fluids. This required the President to lie completely flat. It was very difficult for him to breath. He said he could take lying flat for only a few seconds. They failed to put the line in the first time and then abandoned the attempt.
Ben Aaron was still watching the blood flowing steadily out of the President. “When you see blood coming out of the chest that fast, and that persistently, without letup,” Aaron would say later, “then you have to make some decisions.”
It was now obvious that surgery was the safest course. Was a large blood vessel in the wound ready to burst? Would the blood flow suddenly increase to 600 to 700 cc’s every five minutes instead of the present rate of 300 cc’s every ten to fifteen minutes? Those were the questions preying on Aaron’s mind. He didn’t want to be wheeling a 70-year-old patient who was in shock into the operating room for chest surgery.
Aaron now told the President that he wanted to go in and find the source of the bleeding and stop it. The President said go ahead. Aaron then spoke with Mrs. Reagan and explained options. She too said go ahead. They would operate.
The President had been in the hospital for 30 to 35 minutes.
• • •
If anything, the CT scan of James Brady’s brain was more discouraging than the original X-rays and clinical findings. Dr. David Davis, chairman of radiology at GW and a highly respected neuroradiologist, looked at the scans—three-dimensional sectional views of the interior of the brain—and said he did not think Brady would survive. Besides the widespread bone and metal fragmentation, there was continued brain swelling, and the CT scan had picked up a very large clot developing in the right frontal region. That clot was as dangerous as any of the other injuries, and was contributing to the swelling and intracranial pressure. The scan also showed that the bullet had traversed the brain’s ventricular system—the walls of which make spinal fluid—further decreasing his chances of survival.
There was some talk of not operating at all, but Kobrine and the rest of the physicians in the CT room realized that they had no choice. To save time, Kobrine aborted the CT scans when he had enough information to prepare himself for the operation. He knew that it was crucial to begin as quickly as possible. He now spoke briefly with Brady’s wife, Sarah. He could offer her little encouragement.
As Kobrine rushed Brady to OR 4—one of the neurological operating rooms—he figured Brady’s chances of survival were less than one in ten. As they neared the OR suite, Kobrine was annoyed to see someone being wheeled in ahead of his critically injured patient.
“Who’s that?” Kobrine asked.
“The President,” he was told.
• • •
The President’s stretcher had been wheeled from the ER straight down the hall to the thirteen-room operating suite. He was accompanied by IV poles carrying blood and fluids, and by Secret Servicemen, physicians, nurses, and medical technicians. And at his side was Mrs. Reagan, holding his hand.
Sol Edelstein, the ER director, walked in front of the stretcher to stop it from moving too fast. He was afraid the IV lines could be yanked out of the President’s arm. Another doctor held the President’s foot because the stretcher had no sides. They took a shortcut through the recovery room. The patients there, still groggy from anesthesia, lifted their heads to see what the commotion was about.
David Gens was in his street clothes. He was to assist on a peritoneal lavage or “belly tap,” and didn’t want to take the time to run to the men’s locker area to change into his sterile greens. He went into a small closet near the OR, closed the door, and changed in total darkness. Dr. Ruge, wearing a warm wool suit, removed it, wound it up in a ball, and put it on a window sill when he changed into his greens. Ruge continued to reassure the President that things were going well, that he was in good hands.
There were gawkers. One, a GW staff 118 The Washingtonian/August 1981 member, remained on the telephone in the posting area just outside the OR and talked and talked, refusing to hang up. Finally, Mike Barch, the Medical Center administrator, threatened him with arrest if he didn’t leave. He left. Another gawker, a gynecologist, stayed on and on in the operating room. He just wanted to help, he kept saying. He was finally shown the door.
A Secret Serviceman removed his shoes. He thought it was necessary before entering the OR. “You could tell the Secret Servicemen,” one doctor remarked. ”They all had some part of their OR greens on wrong.”
• • •
The President was taken to OR 2, the cardiac-surgery room with an amphitheater and superb stereo system. Brady went into OR 4 with Dr. Kobrine, and McCarthy into OR 5 with Doctors Tsangaris and Colombani. The three patients arrived at the operating suite at virtually the same time.
The ORs are lined with green ceramic tiles that often give off a hollow sound. Today OR 2 was filled with too many people for that. Many of them were security people.
Stephen Pett, a thoracic surgeon who was in the operating room to assist Aaron if necessary, was asked by a Secret Serviceman to identify anyone he didn’t know. Pett glanced around, then focused on one face.
“I don’t know that guy,” he said, pointing to a tall man.
“That’s the President’s doctor,” Pett was told.
As the President was lifted off the stretcher and onto the operating table, he looked around and, in a move his doctors interpreted as an attempt to break the tension, remarked: “Please tell me you’re all Republicans.”
Dr. Joseph Giordano, a liberal Democrat who was there to do the belly tap, gave a tactful answer. “Today we’re all Republicans, Mr. President.”
Dr. George Morales, a highly respected authority on anesthesiology, continued to attend to the President.
“How are you going to put me to sleep? I can hardly breathe now,” the President said.
Everything would be fine, Dr. Morales assured him.
Assisted by Dr. Manfred Lichtmann, chief of anesthesiology at Walter Reed Army Hospital until he joined the GW faculty, Morales faced the risky problem of putting to sleep a 70-year-old man who was injured seriously and had just eaten, a factor that could provoke vomiting.
Valium was administered, followed by a synthetic narcotic and then Pentothal. As the President was drifting under, Dr. Lichtmann performed what is called the Sellick maneuver: With his fingers, he pressed the cricoid cartilage—a ring-shaped cartilage—on the upper trachea against the esophagus, exerting enough pressure to block the esophagus and prevent any backward flow of food and stomach acid if the President vomited. The major risk occurs if food and acid come up and go into the trachea and are drawn into the lung. In such a case, there is a significant risk of death.
The Sellick maneuver was brought off beautifully, and, with remarkably little Pentothal, the President went under. A tube was introduced into his trachea to permit him to breathe during surgery.
Giordano, Gens, and Wesley Price immediately began the belly tap. Giordano made a small incision just below the navel and inserted a catheter through it into the abdominal cavity, sealed off from the chest by the diaphragm. They poured in a liter of sterile saline solution and then shifted the President’s position in order to wash the fluid around and out. When the cavity emptied they examined it, and it was absolutely clear. The procedure had taken 30 minutes, and they were now 99 percent certain that he had no abdominal injury. To be 100 percent certain they sent the fluid to the laboratory for analysis.
As Dave Gens was closing the abdominal incision, a thought struck him. He looked up at the faces surrounding the President on the operating table and asked: “Does anyone know what’s going on out there?”
There was silence initially. Then Gens was asked what he meant.
“A lot of people were shot,” Gens said. “Is there a conspiracy?”
No one knew. No one had had time to give it much thought.
• • •
For the exploratory operation, Dr. Aaron would be assisted by Dr. Kathleen Cheyney, a thoracic fellow at GW and Aaron’s regular surgical assistant. Dr. David Adelberg, an intern, would also assist. Lula Gore and Thomas Rhodes would be scrub nurses, and Deborah Medenhall and Priscilla Segal were circulating nurses.
Aaron insisted that the President be treated like anyone else. He feared what doctors call the “VIP syndrome,” in which rich or famous people are accorded deferential treatment and usually are much the worse for it.
They turned the President on his right side at about a 45-degree angle and made a six-inch incision along the front and left side of his chest.
Aaron “opened,” and Dr. Cheyney retracted the incision as Aaron cut. The President’s chest muscles were parted and his ribs were spread with a large chrome rib separator. When Aaron first got inside the chest he immediately found a 500-cc clot of blood in the left lower lobe. Now the total amount of blood lost by the President was nearly 3,000 cc’s, about half of his total supply.
The entry point of the bullet was a jagged slit, but as the bullet had moved into the lung tissue it had made a round hole, about the diameter of a dime.
Aaron saw that the blood flowing out of the wound was still dark. Hi; was convinced that part of the pulmonary artery down in the lower lobe had been struck.
He kept exploring. He opened an area near the heart and looked at it. The pericardium had not been hit. The aorta also was untouched. Aaron now began following the bullet track. The bullet had apparently headed on a downward course until it hit the top of the seventh rib and was deflected toward the upper middle of the chest.
He held the President’s lung in his hands, feeling in the soft, spongy material for the hard fragment of bullet he was determined to find and remove. He was as impressed by the texture of the lung as he had been by the muscle tone of the President’s chest. Both resembled those of a much younger man.
“It made sense to take the bullet out of the President,” Aaron later said. “What I wanted was a nice clean operation. I didn’t want to back out and leave the bullet in there.”
But he couldn’t find it.
He kept fingering the lung—squeezing, probing—but the bullet wouldn’t turn up.
Then the fear hit him. Maybe it had gotten into the pulmonary vein somehow. If that had happened, it could have gone into the heart and now be moving out into the arterial tree. That, Aaron knew, could be very serious.
He asked Ruge: How important is it that I get the bullet out?
What’s important is that the President survive, Ruge answered.
Aaron kept looking. Several minutes passed. Tension in the OR mounted.
Dr. Lichtmann, often the anesthesiologist when Aaron performed heart surgery, had seen him in tight spots before. He knew the signs—the knit brow, the tight expression—and he often tried to break the tension with a standard remark. He tried it now.
“You enjoying yourself, Ben?”
Aaron glanced up and smiled for a split second.
Lichtmann and Morales kept monitoring the President’s vital signs. His arterial pressure was good. But the EKG picked up a minor electrical conduction abnormality in the President’s heart. It was a preexisting condition, they were told, and no one became unduly concerned about it.
Aaron called for another X-ray—a side view—to get a better fix on the bullet’s location. The film was rushed down to the lab for developing.
• • •
In OR 5, everything was moving routinely. Paul Colombani, a chief surgical resident, was performing most of the surgery on Tim McCarthy, with Dr. Tsangaris. The bullet had traversed McCarthy’s right lung, diaphragm, and right lobe of the liver.
They found the bullet behind the liver, and when Colombani plucked it out he thought it looked strange. It appeared to have a hollow point, shiny on the inside and copper-colored on the outside. It was hardly deformed at all.
He gave the bullet to a Secret Serviceman who was holding out a cup. Another agent took extensive notes. The news was rushed to OR 2 that the weapon used in the shootings was a .22 caliber, not a .38.
McCarthy’s vital signs remained stable. They were sure he would survive.
• • •
In OR 4, where James Brady lay prepped and ready for brain surgery, the story was quite different: A life was hanging on the edge. Dr. Kobrine looked at the CT scans a final time to consider his options and decided on a coronal opening. This is an ear-to-ear incision over the top of the head. Kobrine thought it would afford the best possible exposure. The operation began less than an hour after Brady was shot.
There was concern about Brady’s left eye. The swelling was so pronounced that it was putting pressure on the eye. Dr. Mansour Armaly, an ophthalmologist on the GW faculty, made a small incision to drain the clot on the eye.
As he peeled away the scalp, Kobrine could see the bullet hole through the skull. It was less than a centimeter in diameter. (To this day, Kobrine is uncertain whether the bullet—later identified as a “devastator”—exploded on impact. It probably didn’t, nor did any of the others.) Kobrine saw that the bullet had gone through the sinuses and realized that this would greatly complicate Brady’s recovery if he survived. The injury there created a direct air passageway to the brain that could lead to infections.
A saw was used to cut the skull and expose the brain.
Kobrine initially focused his attention on an opening made by the bullet in the dura, the outermost membrane covering 120 The Washingtonian/August 1981 the brain. He widened it to work down deeper into the left frontal lobe, from which he cleaned out the bone and bullet fragments and removed dead tissue.
One of the several doctors shuttling between the operating rooms and the second-floor offices where hospital and White House officials waited popped his head into OR 4. “The networks report that Brady is dead,” he said.
“No one has told Mr. Brady or me that,” Kobrine replied without looking up.
Neurosurgery is called the queen of surgery because such precision is required. Wearing a microscopic lens, and illuminating the small surgical field with a high-intensity light attached to his forehead, Kobrine moved quickly but delicately. Brady’s intracranial pressure remained very high.
Kobrine now moved to the right side, where he made a large opening through the dura to suction out a small hematoma near the surface.
Suddenly something entirely unpredictable happened—something that in great part is the reason Brady lives today.
Deep within the right side of Brady’s brain, a large blood clot—the same clot that was so worrisome when Kobrine saw it on the CT scan—spontaneously burst. It could have been a catastrophe. Instead it was a godsend.
Its force was so great that it gushed up and through Brady’s brain tissue, literally creating a fountain of blood when it broke through the brain’s outer surface. If someone could have selected a place for that clot to burst its way out of Brady’s brain, it would have been in the right frontal lobe, precisely where it did. This is one of the less important areas of the brain, especially for someone who is right-handed. The bursting of the clot opened up a world of possibility unthinkable only moments before. It decompressed the potentially fatal pressure buildup within Brady’s brain. His excessively high blood pressure returned to normal.
The opening made by the bursting also provided Kobrine with an unobstructed access route down into the brain. From this he was able to retract the right hemisphere and control two major damaged vessels with silver clips and electrified forceps. One of the vessels was the anterior cerebral artery, which had been severed by the bullet. He then slipped his finger into the opening and felt the main fragment of the bullet, which he extracted with forceps.
There was still much to be done, and Brady remained in critical condition. But something close to a miracle had taken place.
• • •
The President’s chest X-ray indicated that Dr. Aaron had been looking too low for the bullet. Now he put a catheter into the bullet track and began to follow the path. Minutes passed. He thought of closing the chest and leaving the bullet inside, but decided to stay with it a while longer.
Finally, his fingers felt something hard—the bullet. Sounds of relief filled the room as Aaron removed it by carefully squeezing it out through the lung tissue.
Now he knew why it had been so hard to find: It was flattened to the size and shape of a dime. It was thin at the edges, thicker in the middle. Rifling marks were still evident on the edges. As before, a Secret Serviceman extended a cup for the bullet. As before, an agent took copious notes.
The bleeding from the wound had finally stopped, and Aaron left a drainage site where he removed the bullet, irrigated the wound area, and began to sew over it, having made certain no major section of the pulmonary artery was damaged. It was now calculated that the President had lost about 3,300 cc’s of blood. Two tubes were left in the President’s chest; one at the top for air retrieval, one at the bottom for drainage. Now, more than three hours after the President entered surgery, the doctors began to close his chest.
• • •
There was some debate as to where the President should spend the night—the intensive-care unit or the recovery room. Aaron wanted him in the recovery room. It was near the operating suite and, in the case of complications, provided quick access to the OR.
Shortly after 6:30 in the evening, the President, still breathing through the endotracheal tube, was wheeled across the hall into a comer of the recovery room, which has a capacity for several patients.
Ben Aaron’s day wasn’t finished. Now he was called to examine another patient—one he’d operated on recently for a heart-valve replacement—who was bleeding. One look at the patient and Aaron realized he had to go back to the OR. All in all, he would spend 14 hours in surgery during a 24-hour period from midnight Sunday to midnight Monday.
• • •
George Morales returned to his small office in the anesthesia area near the OR suite. He found it filled with communications equipment. On his door a makeshift sign read: TEMPORARY WHITE HOUSE.
• • •
A curious phone call was received by a physician at GW. It was from an associate of Dr. Michael DeBakey, the noted Houston heart specialist. He said Dr. DeBakey and members of an emergency team would be willing to fly to DC immediately to help if GW would agree.
The call was interpreted in two ways. A few GW doctors considered it an honorable offer of aid in time of national crisis. But most GW doctors considered it self-serving. Said one: ”The call was the height of arrogance.”
The offer was refused.
• • •
After receiving a thorough medical briefing from Aaron and other doctors, Dennis O’Leary, dean for clinical affairs, left his hospital office to brief the nation at a press conference. He and Dr. Ruge were the major candidates for the spokesman job, but Dr. Ruge declined, saying he thought there might appear to be a conflict of interest if he took on the role. He said that someone from the hospital ought to speak for the hospital.
Darkness had fallen when O’Leary crossed 23rd Street on his way to Ross Hall, where he was about to address the nation via TV and radio. As they walked, presidential aide Lyn Nofziger said:
“Remember, you don’t have to answer a question just because someone asks it.”
O’Leary’s explanation of what had happened would deliberately de-emphasize the dramatic and accentuate the positive.
• • •
The lung is a gas exchanger. From the pulmonary artery, blood flows into it laden with carbon dioxide. In the small vessels and capillaries of the Jung tissue, the carbon dioxide is exchanged for oxygen extracted from air we inhale. During this exchange the blood turns from a dark, ruby color to a bright red, ready to bring oxygen out to every tissue in the body.
As the world was hearing that the President had sailed through surgery, the many specialists surrounding him in the recovery room were considerably more guarded in their optimism. The President’s first post-operative X-ray showed white shadows that indicated pockets of airlessness in the lungs. It also showed considerable plugging of the small sacs and vessels from secretions. Toward the bottom of the film there was a shrunken, whitish area where blood had pooled. The X-ray also showed that the left lower lobe was collapsed. To some’ of the doctors the X-ray findings were’ worrisome; they could not understand why the lower lobe was collapsed. To others the collapse as well as most of the other complications were predictable and not alarming.
But a finding that concerned all of the doctors was the level of oxygen in the President’s blood, a measure of his lungs’ gas-exchange process. The lab analysis showed it wasn’t working well. His blood’s oxygen level was normal only when the respirator was giving him 80 percent oxygen—compared to 20 percent in normal air. Several doctors became openly concerned. They began taking readings every few minutes simply by drawing blood out of the arterial line in his wrist.
The respirator was set to give the President something called PEEP, an acronym for positive end expiratory pressure. This allows the respirator to trap gas in the lung at the end of each breath to open up and prevent the collapse of lung airways.
The President was not yet conscious. He lay on the stretcher, with the endotracheal tube down his throat. He was hooked up to an EKG monitor, blood pressure and pulse monitors, and IV lines. His head was tilted up at 30 degrees and he was surrounded by a small army of medical personnel, Secret Servicemen, and some of his aides, Baker and Meese most prominently. The aides asked when the President would be able to make decisions but didn’t receive a precise answer. One other patient was in the recovery room at this time, and the President’s bed, facing the wall in a far comer, was cordoned off with screens. Secret Servicemen stood at every entrance.
The President began to regain consciousness at about 7:30 PM, and he indicated that he felt he couldn’t catch his breath. It is a sensation many people on respirators experience, and it can be frightening. He was assured the respirator was doing his breathing for him.
Between 7:30 and 8 the President’s wife and their son Ron visited briefly. They held the President’s hand. Mrs. Reagan kissed him, and Ron leaned over and whispered into his ear. Although he was aware of their visit, the President remained groggy. Mrs. Reagan expressed the President’s concern—and her own—that he felt he could not breathe. It was an advocate’s role she was to play throughout his stay in the hospital and one that at times exasperated the President’s doctors. But they understood her concern and patiently tried to keep her abreast of developments.
Mrs. Reagan was now reassured that the President was breathing as he should with the respirator and, at the doctors’ urging, she prepared to leave. Before doing so, she stood alone in the open doorway of the recovery room for what seemed like minutes and looked back intensely at her husband’s bed, the worry plain on her face.
At about 8 PM the President experienced pain and was given morphine. He most of the President’s drugs (and meals) were brought over from the White House. Secret Service agents randomly selected other drugs from the hospital pharmacy.
Dr. Ruge remained in the recovery room that night—and, in fact, would stay at the hospital around the clock until the President was discharged. His role there was important not so much for what he did Dr. Ruge intrude, impose his judgement, or demand that outside consultants he brought in to examine the President. He was obviously in the spot to do that, and it might even have afforded him some protection from second-guessing if he had. But he had confidence in the GW doctors and they in turn trusted him.
“Never once,” Dr. Ruge would later say, “did I consider bringing in outside consultants.” Nor did Dr. Ruge consider moving the President to Bethesda Naval Hospital, which was suggested by the Secret Service.
Ruge’s attitude helped avoid the VIP syndrome—of acting so deferentially that a patient is taken out of the normal hospital routine. That evening two chief surgical residents, David Gens and Paul Colombani, were assigned to take continuing care of the President. Although some physicians at GW felt this was a mistake, that a large team of senior specialists should have been assigned full time to this patient, the more standard approach was taken. “Medicine by conference would have been the worst thing we could have done,” one of his doctors said later. The President was, in the words of another of his doctors, “treated like any other 70-year-old man with a gunshot wound.”
Different doctors focused on different things during those first few hours in the recovery room. Dr. Samuel Spagnolo, pulmonary-medicine specialist, fixed on the rhythmic beeping and the steady line blipping across the screen of the EKG monitor. In all the hours Spagnolo watched, the President’s heart didn’t miss a single beat.
Sol Edelstein marveled at the powerful muscles in the President’s chest, developed from outdoor work. Dr. Ruge said he’d seen the President toss around ranch posts as though they were bamboo sticks.
They now took another blood-gas reading, and the results were no more encouraging than the earlier ones. More X-rays were taken, and they showed the lower lobe still collapsed. There was concern that the President might have to stay on the respirator for up to three more days unless there was quick improvement. To keep him on 80 percent oxygen would invite other problems for his lungs.
A wounded President attracts medical voyeurs. In the recovery room that first night a short man dressed in a suit marched in and went directly to the President’s bedside, where he leaned intently over the President. How he breached security is uncertain. He had absolutely no business being there. One of the doctors peered at him and asked in a loud voice, “Who the hell is that guy?’n Others also looked with curiosity at the short man. Dave Gens, who recognized him as a doctor—a part-time GW faculty member—told him, politely, to leave. He refused. Then Mike Barch, who was helping the Secret Service screen people, approached and asked what business the doctor had there. The doctor told him he had a patient in the hospital. Barch went to the phone and checked. The doctor had no patient at GW. Barch had hospital security officers escort the doctor out of the building.
The President was handed the back of a hospital progress sheet attached to a clipboard to write on. And write he did. Early notes continued to express his worry over his breathing, but their tone lightened at times.
“Am I alive?” he asked in one after waking from a brief nap. Another said he’d like to shoot the whole scene over, beginning at the hotel.
Because his lungs were so congested, there was an attempt to perform a bronchoscopy. This involves slipping a fiber optic tube down into the bronchi and clearing out clotted blood or other debris. The attempt failed because a bend in the endotracheal tube blocked the bronchoscope’s passage.
Jack Zimmerman, the director of the intensive-care unit and considered one of the best clinicians at the hospital, had come to the recovery room to assist. When the bronchoscopy failed, he had nurses Denise Sullivan and Kathy Edmonston take a small volume of saline solution and insert it into the endotracheal tube. It caused the President to cough, freeing mucous plugs and thinning out secretions, which were then suctioned out. In the midst of this the President wrote the note that echoed W.C. Fields: “All in all, I’d rather be in Philadelphia.”
Most doctors and nurses took the note writing to be a reflection of the President’s exuberance at being alive and as his way to break the ongoing tension.
The notes kept coming. One to Denise (Denny) Sullivan, the head recovery-room nurse, read: “Does Nancy know about us?” The Secret Service took that note and all the others the President wrote.
Then came a different kind of note: “Was anyone else hurt?”
Denny Sullivan, a bright, quick woman with fifteen years of nursing experience, froze for half a second and thought quickly. Two others were hurt, she told him, but not seriously. She had not heard of the fourth victim, Officer Thomas Delahanty, who had been successfully operated on at the Washington Hospital Center for a wound to his upper spine.
Then another note: “Did they get the guy?” Yes, Denny Sullivan told him, they did.
Dr. Ruge then conferred with the medical staff. There was agreement that if the President asked again, he was not to be told of the seriousness of the injuries to the others, particularly Jim Brady. Considering the President’s condition, an emotional jolt was too much of a risk.
A new blood-gas reading was taken, and it showed improvement. The news was greeted with relief, and joy.
• • •
Tim McCarthy had been taken directly from the OR to the intensive-care unit for post-operative observation. He was doing extremely well; his vital signs were strong and stable.
• • •
Toward 8:30 PM the six-hour operation on James Brady was ending. Dr. Kobrine had no certainty that Brady would ever be able to function again, but he was more encouraged now than he had been before surgery. Brady was wheeled into the recovery room at about 9, and Kobrine went to look for Sarah Brady.
• • •
Optimism took hold as the President’s blood-gas level continued to improve. The oxygen from the ventilator was slowly reduced as his blood oxygen slowly increased—which meant his lungs were resuming function.
He remained surprisingly alert and continued to write notes. “I don’t think I’ve ever seen a person that age with that kind of injury do that well,” Zimmerman later said of the President’s recovery-room performance.
As the hour neared midnight it was becoming clear that if improvement continued the President could be allowed to breathe without assistance before daybreak.
He apparently became unnerved momentarily when he overheard Ben Aaron describing to other doctors the condition of the heart patient he’d treated after he’d operated on the President.
“Is that happening to me?” the President wrote.
Marisa Mize, the recovery-room nurse, who had come on at 11 PM for the night shift, quickly reassured him that it wasn’t. An attractive, lively woman of 26, she sat next to the President for long periods of her shift—holding his hand, talking to him. At one point she rose to leave. The President seized her hand. His look told her not to go. She sat back down next to him.
At times she kidded him. “Don’t worry,” she said to him once, “your wife isn’t holding dinner for you.”
“I’m not that hungry, anyway,” he wrote.
• • •
At about midnight James Brady began slowly to come out of anesthesia. Small tremors rippled over his body—a good sign. Often in cases of serious brain damage the patients do not have these post-anesthesia tremors because the neurologic damage is so great.
Another good sign: Brady started to move one of his toes. And then a nurse insisted that he had squeezed her hand.
Kobrine had realized during surgery that Brady’s left side was not going to be as good as his right. The right hemisphere of his brain had taken most of the damage, and it controls the left side of the body. Also, the major vessel damage was to vessels that led to areas of the brain involved in motor function. It became clear watching him in the recovery room that the motor functions of Brady’s left side were substantially damaged.
But Kobrine found another hopeful sign. The swelling around Brady’s eyes had now abated enough for Kobrine to put a light to them, and he found that, happily, they were not fixed and dilated.
Post-operative CT scans were now taken and they showed marked improvement over those taken just before Brady was wheeled into surgery.
Maybe he’s going to do better than we all anticipated, Kobrine thought.
• • •
At 1:30 in the morning the President thought it was 6:30 in the evening, but other than that, he was experiencing little disorientation. Doctors explained to him what had gone on in the OR. He was now given morphine for pain, but his blood gases came closer to normal.
Slowly and carefully the attending physicians began to wean him from the respirator, and, as they did, he began to “buck”—to get out of sync with it. He started coughing and became agitated.
At approximately 2:30 in the morning the President had another scare. As doctors began removing the endotracheal tube, they kept saying, “This is it, this is it,” meaning that the time had come to take him off the respirator.
Marisa Mize saw the fright in his eyes. “What do they mean, ‘This is it?”‘ the President scribbled.
She explained and he calmed down.
By 2:45 AM the President was off the respirator for the first time in nearly twelve hours. He had an oxygen mask on but was able to speak. His voice was hoarse.
He immediately expressed concern for the others who were wounded and asked about the motives of the assailant.
No one in the recovery room dared to say anything about the other victims.
Although tired, the President continued to talk with his doctors, nurses, and aides. They soon realized he had a partial hearing loss in his right ear that predated the shooting. By 4:30 the recovery room had pretty well thinned out, and several lights were turned off so the President could sleep. Joanne Bell, a recovery-room nurse, put a gauze pad over his eyes to block the light and moved away to let him sleep. Within seconds he had the pad off and was talking again. She walked back to the President’s bed, took the pad in her hand, and said: “Mr. President, in the most polite way I can tell you, when I put this over your eyes, that means I want you to shut up.”
He looked up at her, winked, and took a 45-minute nap.
Ben Aaron went to sleep on a stretcher. Gens and Colombani found beds in the kidney-dialysis unit, but it was so hot that Gens woke up at 3 AM and returned to the recovery room, where, with Zimmerman, Spagnolo, Edelstein, and Price, he stayed until early morning.
At approximately 6:15 Tuesday morning the President was wheeled from the recovery room to the intensive-care unit (ICU) on the fourth floor. His room’s curtains had been drawn. Although small and nondescript, the room was crowded with people and medical equipment.
The ICU nurses now began giving him respiratory therapy, which consisted of having him cough and breathe deeply, and of pounding him on the back.
Carolyn Ramos helped the President brush his teeth and then she brushed his hair. “Now you can tell everyone I don’t dye my hair,” he said. Indeed he doesn’t, a fact that his nurses and doctors can confirm and one that, to their surprise, several members of the President’s staff took pains to point out.
What also surprised those who took care of the President was his ability to put them at ease—to kid with them, talk with them, to give them the impression that he was a totally accessible and secure man. Republicans and Democrats alike came to admire him.
In the ICU, where the President was to remain that day, Carolyn Ramos felt enough at ease to joke with him. Sometimes, she told him, patients who have undergone surgery are asked questions to determine how oriented they are. Typically, she said, they are asked the year, their whereabouts, and the name of the incumbent President. “In your case,” she said, “we’ll skip the last question.”
The President laughed.
Then she told him that a recent patient, when asked who the President was, said: ”That actor fellow… Jimmy Stewart.”
He laughed again.
The President’s aides visited early that morning, a practice they would continue throughout his stay at GW. The President said to them that he’d known that missing a staff meeting would be too much to hope for.
The same morning the President signed into law a bill eliminating a scheduled increase in dairy price supports. He’d been given a total of 30 milligrams of morphine for pain over the last several hours, and some of the nurses wondered how a man who’d taken that much morphine could understand what he was signing. They kidded among themselves that they should put the student-loan bill in front of him to sign.
The President showed a persistent curiosity about who had shot him. And although he seemed satisfied when told that the others were not hurt badly, he continued to ask about them too.
Later that morning Dr. Ruge finally told the President about the seriousness of the injuries to James Brady and the others. He appeared deeply shaken by the news, and said he felt guilty because he realized he had been the target but that others had to suffer for it. He didn’t need a supporting cast, he said. That morning Dr. Ruge talked to members of the Cabinet and spoke very optimistically of the President’s condition.
The President’s room in intensive care became oppressively hot because of the large number of people now gathered there and because it was unseasonably warm and the hospital’s air conditioning was not yet turned on. Nancy and Ron Reagan visited in the morning; Maureen came in the afternoon. Mrs. Reagan wanted him moved as soon as possible. But because the suite on Three South that he was to occupy had yet to be prepared and made secure, the President had to wait all day in this little room in intensive care.
That afternoon X-rays of his lung showed that his left lower lobe, which had collapsed after surgery, had fully expanded. But he was in pain, and was given codeine.
The next day, Wednesday, it was decided to cut back sharply the number of medical people with access to the President, in part because the President and Mrs. Reagan were being made uncomfortable by people in such number in such a space.
Ben Aaron, pulmonary specialist Sam Spagnolo, and Gens and Colombani, the chief surgical residents, were to be the only physicians with direct access. It would be Gens and Colombani, both in their 30s, who would write the President’s chart, give him his IVs, draw his blood, change the dressings on his wound, and otherwise look after him on a day-to-day basis. Dr. Aaron was in overall charge. Dr. Ruge, still the President’s physician, kept Reagan informed of developments. They would all meet early each morning to examine the President and then, after the chest X-ray was taken, would confer with Dr. Rockoff, head of chest radiology. Later that first week, the list of GW doctors with direct access would be narrowed further, with Dr. Spagnolo acting as a consultant.
By 9 PM Tuesday, the President’s second night at GW, the Three South hallway was secured and turned into a miniature presidential compound, with a sitting room for Mrs. Reagan, a room for Dr. Ruge, two rooms for Secret Service agents, and a conference room. The President’s room had two easy chairs and a sofa, and a Secret Serviceman was there at all times. The windows of this room were bullet-proof.
Although chest-surgery patients are normally kept on the sixth floor, the Secret Service did not want the President on the top floor, for security reasons. In every move the President made at the hospital, the Secret Service took all security precautions, checking hall s, doors, anything that could present a problem. The agents moved quietly and efficiently through the hospital, their identity made clear by the small button in lapel and bulge under jacket. The hospital staff realized that some carried Uzi submachine guns in their benign-looking briefcases. A SW AT team remained on the hospital roof. All hospital entrances except the one on 23rd Street were sealed.
The Secret Service agents, the doctors and nurses said, were unfailingly courteous and professional. They came to be greatly admired by the GW staff.
• • •
With the President’s arrival imminent, Sylvia LeBlanc, a young nurse on duty at Three South, felt her hands growing cold and clammy. She knew that she’d have to pound the President’s back as part of his respiratory therapy. She decided to wash with warm water—just before the therapy—because she wouldn’t want to hit a President with cold hands.
That first night in Three South was uneventful, but in the early-morning hours of Wednesday Dr. Colombani realized that the President had not urinated since the Foley catheter was removed Tuesday afternoon. Colombani had no choice: He woke up the President and told him he’d have to get out of bed and walk around. Colombani hoped the movement would stimulate urinary output. It didn’t. Now Colombani was faced with the unpleasant task of telling the President of the United States that the Foley catheter would have to be reinserted.
The President is a friendly man who had dealt cheerfully with most of his medical problems, but he did not cheerfully accept the news Colombani now had to give him. Gens and Colombani took alternate nights on the presidential watch, and it became a running joke between them that the bad things always happened on Colombani’s shift.
In general, the President’s recovery continued to go exceedingly well. However, while reexamining the President’s abdominal X-rays, Dr. Rockoff saw an abnormality that disturbed him. It was not in the chest but in the back. What he detected was a small, gray shadow on a vertebra in the President’s lower spine—a lesion of some kind, about the size of a pencil eraser. He was unsure of what it was, and there was some fear it might be malignant. This information was shared with very few doctors. They did not tell the President what had been found. They wanted to study it further.
The President continued to cough up blood, but it was dark blood, a natural consequence of his injury. Dave Gens told the President, who was concerned about it: “It’s good—you’re coughing up old blood.”
“Don’t you know what they said about me during the campaign?” the President answered. “I’m full of old blood.”
The one-liners kept coming. And the President did a remarkably good Jimmy Stewart impersonation.
“Mrs. Reagan expressed concern because the President was still occasionally disoriented about time. Gens explained to her that many patients sealed away inside a room with the curtains drawn and without clocks lose track of time.
Assistant Secretary of State William Clark, longtime friend of the President’s, was there complaining that he’d just had a terrible day on Capitol Hill. He said he felt useless and he wanted to do something to feel useful, so he’d buy the President a clock.
He did. A big Mickey Mouse clock hung in the President’s room for the remainder of his stay.
That first Wednesday, the President’s blood-oxygen level dropped dramatically. He was immediately put back on oxygen, now given to him through nose prongs instead of a mask. IVs still came into his arm. A picture of the President and Mrs. Reagan, taken that first week, showed the President smiling as he stood in his robe. Cropped out of the picture was a nurse, standing to his immediate left, holding the Pleur-evac connected to the chest tube which came out from under his robe. Mrs. Reagan was very particular about that photo: She did not want her husband to be pictured as an invalid.
Forty-eight hours after surgery, the President was taken off precautionary antibiotics. Standard procedure. He had an emotional visit from Sarah Brady. He expressed sorrow and she told him that her husband was doing better, that she was hopeful. Every night when Dr. Ruge came by, the President would ask how Jim Brady was doing. When Dave Gens arrived back in the on-call room across the street from the hospital late that Wednesday night, his first night on the President’s watch, he sat on the bed for a few moments and realized that with all the security arrangements it would take him three or four minutes to get back to the President’s bedside if there was an emergency. Too much time would be lost.
He promptly got up, walked back to the hospital, and went to sleep on the sofa in Mrs. Reagan’s sitting room, adjacent to the President’s room. He did this every night he was on duty. He made certain, however, that he was always up very early. He didn’t want to be caught sleeping in the First Lady’s room.
Thursday morning, April 2, the abdominal stitches from the President’s peritoneal lavage were removed, and it was learned that a “devastator” bullet had been used by the assailant. Hurried calls were made to determine if lead azide, a component of that type of bullet, was dangerous. An authority in Colorado assured the GW doctors that it was not.
The President had been awakened twice each previous night, for respiratory therapy, and it was now decided to let him sleep through. His spirits were high. He still kidded with the nurses and doctors, watched TV, and read everything he could about his shooting. He seemed to prefer entertainment on TV, one night passing up a documentary on El Salvador to see The Birds, an Alfred Hitchcock movie. He continued to confer with his aides—Meese and Baker, among others—daily.
On Thursday night the President’s splendid recovery came to a halt—a worrisome fever was detected. His temperature ranged between 102 and 103, and was soon accompanied by other problems. Tylenol helped somewhat, but the moment its effects wore off, the fever would peak again. His color worsened and he became more tired and less gregarious. His white count went up. Colombani, on duty that night, called Ben Aaron at home, late. Aaron said to continue with the Tylenol. The President’s one remaining chest tube was examined as a possible infection source. It was “clean.” The few people who knew about the fever were disturbed by it. It was a setback.
• • •
On that same Thursday night a different drama was unfolding at the Washington Hospital Center. The FBI, which had earlier misled the Secret Service about the caliber of the bullet used in the shooting, said it had now learned that “devastator” bullets had been used and thus informed the physicians who were treating DC policeman Thomas Delahanty. Told of this, Delahanty gave his permission to remove the bullet, which was lodged in the region of his upper thoracic spine.
In a delicate two-and-a-half hour operation, neurosurgeon Dr. Michael Dennis (not wearing a flak jacket, as widely reported) removed the bullet. Although there was some fear that the bullet could explode, the greater fear was that it might release a caustic chemical.
In the wake of the shootings at the Hilton, some members of the DC police department were angered over what they considered the FBI’s hunger for publicity. Some police officers hinted that the FBI had deliberately tricked Delahanty’s physicians into removing the bullet—not for any medical reason but for evidence. There is no basis to suspect this is true.
• • •
Blood, urine, and sputum cultures were negative. The President’s fever continued through Friday, and on Friday night he began to experience chills. He asked about the source of the new problem, but no one knew what was causing it. The daily X-rays continued to indicate that there was some fluid in the lungs, which could mean pneumonia. Concern about his condition grew. Aaron decided to do a bronchoscopy to try to clear up the bronchial tubes. To prepare a patient for a bronchoscopy, a spray solution of Xylocaine is used to deaden sensation in the throat, and often Valium is administered to relax the patient. Edward Yob, a White House physician, approached Dave Gens and asked if Valium was going to be used. Gens said it probably was.
Yob asked if they could hold off giving the President major sedatives. Gens asked why. Yob said he dido ‘t know but something very important was going on in the world and unless it was absolutely necessary to sedate him, the President was to be kept fully alert. Gens never learned the nature of the crisis.
While the doctors were preparing for the bronchoscopy, a procedure that if done openly would alert the hospital staff that the President was sicker than generally realized, the decision was made to keep it a secret. Problem: The bronchoscope is carried in a black case with the word OLYMPUS—the manufacturer—printed in large letters on the side; anyone who saw one of the President’s doctors carrying it would know what was going on.
When Gens went to the pulmonary department to get it, the nurse routinely asked him for the patient’s card so she could add the treatment charges to the bill. Gens has a hard time lying, but he did.
“I forgot the card,” he said apologetically. “I’ll bring it tomorrow.”
He took the case, put white tape across the word OLYMPUS, and carried it to the President’s room.
Valium was not necessary. Aaron suctioned out some old, clotted blood with the bronchoscope, and, through the eye piece, viewed the bronchi. He found no pus or other sign of infection.
There was no change in the President’s fever that night. His appearance and spirits continued to sag. One doctor remarked to another, ”The President looks terrible.” President Reagan’s fever was being described to the public as “moderate.” There was no public hint that his doctors thought it possible that he had a lung infection.
On Saturday, five days after the shooting, another complication developed. The President had been coughing up blood all week, but the color was dark—it was obviously old, clotted blood and thus not alarming. However, the color of the blood he coughed up Saturday morning was bright red—fresh blood. Taken in combination with the fever and chills, it was “an ominous sequence of events,” Aaron said later. The President had been put back on his original antibiotics, but to no avail. The fever persisted. So did the red blood coming up.
Aaron told Dennis O’Leary and Dr. Ruge Saturday that he thought the President was very vulnerable, that the new blood coming up could be a prelude to a major lung bleed. At one point, Aaron considered the possibility of going back in and surgically removing the left lobe, the source of the President’s problem.
“It was a terribly depressing time,” one doctor recalls of that period. “The President was a lot sicker than most people realize.”
Aaron was more worried about the new bleeding than the fever. But at about the time his worry was deepening, the bleeding stopped. He suspected that a small clot had let go, causing the bleed; at any rate, he was relieved of the risky task of operating a second time.
Yet the fever persisted. What was causing it? No one knew for sure. During the many meetings the physicians had about it, opinions of internists and surgeons divided sharply.
The head surgeon, Aaron, held that the fever was a result of an inflammatory process, a natural consequence of the injury. Gens and Colombani agreed.
Internists such as Spagnolo and Rockoff had a darker worry—that the President had developed an abscess within the lung. If this proved to be the case, surgery might be required to remove it.
These two factions continued to disagree—not angrily but firmly. The surgeons argued that they were seeing the President daily and that he did not appear to be seriously ill. Rockoff at one point countered by saying, “I’m here to keep you from getting too optimistic.”
That same Saturday there was good news. A new series of small X-ray pictures called tomographs gave a detailed picture of the suspicious shadow on the President’s vertebra. Rockoff now determined that the suspicious lesion was not invading the bone, as cancer would. The diagnosis was that it was sclerotic in origin—benign.
Rockoff, who had downplayed the possible significance of the shadow on the vertebra in discussions with the President, now told him that everything was fine. The President looked wearily at Rockoff and said of this latest series of X-rays: “Could we make picture postcards out of them so I can send them to my friends?”
The fever continued. A pivotal meeting was held early Sunday morning in Rockoff’s radiology office. Besides Rockoff, physicians on hand were Gens, Colombani, Ruge, O’Leary, Aaron, and Carmelita Tuazon, director of infectious diseases at GW. When they reviewed the week’s X-rays of the President’s lung, they noted that those taken on the large, stationary machine were of a much higher quality than previous X-rays and revealed the lung densities clearly. Whether these densities had been there earlier or were new was not the major question. The major question was what could be done to get rid of the fever.
Disagreement was voiced, but the tone of the meeting was somber and purposeful. Dr. Tuazon, who had not been called in to consult until Sunday—a day or two too late, some doctors complained—had studied the sputum slides and the blood and urine cultures and suspected that the President had a bacterial infection.
After discussing a number of treatment possibilities, the consulting physicians decided to take the President off his present antibiotic and put him on two new ones, penicillin and amino glycoside, in order to deal with the suspected bacterial infection.
They waited Sunday and Monday for the fever to break; it didn’t. On Tuesday, eight days after the shooting, there was a little optimism because the President’s peak temperature was lower than it had been for several previous days. It dropped further on Wednesday. Gens and Colombani now plotted a temperature curve and boldly predicted that his fever would be gone by Friday. They were off by a day—it ended Thursday. The President looked better, felt better, was better. The crisis had passed.
What caused the fever is still a mystery. Some of those who treated him insist that infection caused it; others say the source was merely post-operative inflammation. Those who think infection was the source say that antibiotics broke the fever; others insist that it would have gone away on its own.
On Thursday of the President’s second week at GW, he was doing so well that some thought was given to taking him off penicillin. But Dr. Tuazon, wanting to take no chances with a possible infection, dug in her heels and insisted that he remain on penicillin for another ten days. He did.
The President’s strength continued to return. Ben Aaron noticed the change: “He slowly emerged from being the perfect patient to a restless man, anxious to get back to work.”
ln high spirits, the President made a practice of walking “laps” in the hallway and telling Maria Blaz, one of his nurses, how many he had done each time he approached the nurses’ station. Once, after he had done three, he turned to her and called: “That’s eight.” She glanced up to catch him smiling.
Blood, urine, and sputum cultures continued to be negative. The patient was almost healthy enough to be discharged.
• • •
James Brady’s condition was improving. He was responding to questions, remembering details about his life, and showing a sense of humor. Moreover, mobility on his right side had improved significantly. His left side showed little motor movement, except for some in his hip.
• • •
On Saturday morning, April 11, all the physicians involved in the President’s treatment met for a last time, in Rockoff’s radiology office. The President’s X-rays were very encouraging; his lungs sounded and looked better. He would remain on intravenous penicillin one more day and then be switched to oral. There seemed no further need to keep him at the hospital. They decided to discharge him that morning.
Gens and Colombani, the doctors who had the most contact with the President while he was at GW, went to his room to say good-bye. The President shook their hands and thanked them warmly. Gens, who had spoken often with Mrs. Reagan during the President’s twelve-day stay, joined Colombani in seeking her out. They found her in the corridor talking with Sarah Brady. She thanked them, hugged them, and kissed them on the cheek.
Doctors and nurses were asked to line up in the hallways so that they could wave to the President as he left. As he was heading out, at about 10:30 that morning, he kept stopping and reaching out to touch or shake hands with the people who had cared for him. Many were touched by his warmth. At the 23rd Street entrance, the President, wearing a cardigan sweater over his bullet-proof vest, said his good-bye: “From the time we came here, in confusion, until now, you have made us all welcome. God bless you all.”
• • •
There are a number of lingering questions about the health of the men who were shot down at the Washington Hilton, particularly James Brady.
Although brain tissue heals very slowly, it appears that Brady’s short-term and long-term memories are intact, and every day his cognitive ability, speech, sense of humor, and zest for life—to say nothing of zest for gourmet food—seem to grow sharper. He will probably never regain full use of his left side—particularly his left arm and hand, which were more affected by his injury than was his left leg. It seems reasonable to assume that, after physical therapy, he might one day walk with the aid of a cane, and that he may have to hold his left arm in a sling.
The President will always have some fibrous tissue in his injured lung, but it is unlikely that he will ever feel any residual effects from it—such as shortness of breath after exercise—once he fully reconditions himself. The only potential long-range problem—and it is very remote—is the possibility of hepatitis from his transfusions. He will probably experience some pain now and then from the wound, but that should ease off when it is fully healed. Doctors assured Mrs. Reagan that the President’s physical activities will not have to be curtailed once he recovers completely.
Tim McCarthy’s doctors also are optimistic. They predict that the Secret Service agent should not face any significant after-effects from the shooting. He is already back on the job.
DC policeman Thomas Delahanty—treated at the Washington Hospital Center rather than at GW—is likely to experience residual pain because of nerve damage to his upper thoracic spine. In addition, says his doctor, Michael Dennis, Delahanty will probably experience permanent numbness on the inside of his left arm.
Several days after the President’s release, Aaron, Gens, and Colombani went to the White House to make a house call. They were ushered upstairs to the President’s working office on the second floor.
Ronald Reagan greeted them by holding out his arms in the fashion of a man accustomed to having needles inserted, smiled, and said, “Here, is this what you guys want?”
They laughed, examined him, and found him well.
This article appears in the August 1981 issue of Washingtonian.