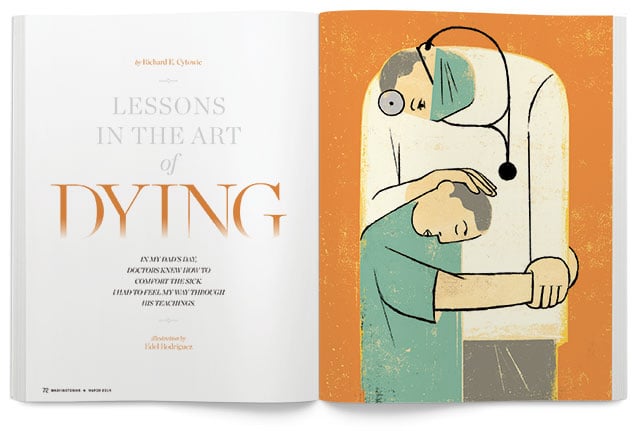
Bethany Howard is a 35-year-old mother of two with a hundred things on her mind. Her iPhone twirling in her hand, she sits across from Dr. Bernard Nash, her internist of 11 years. The doctor sits close, face to face with his patient.
“I’m afraid the news is not what we had hoped,” he says. “The cancer is back.”
Bethany gasps. Her hand flies to her face. Her color drains. As the physician’s words sink in, the logistics of school, dentists, and dance lessons scatter from her mind to make room for the only thing that matters now.
Dr. Nash hates this. After years in medical practice, he’s still uncomfortable talking about death. The silence hangs between them, but he resists the urge to break in. He waits. And then some emotional clutch in Bethany engages. She trembles. Her color returns, overshooting from white to red.
Nash reaches toward her. “I know this is hard,” he says. “It’s hard for me, too. The cancer has moved to your spine, your liver, and your ribs.”
Bethany heaves, tears now spilling down her face. It has been four years since the original lump, the double mastectomy, the chemotherapy. Four years since she returned to work, to her women’s group at church, to the semblance of a normal family life. During her remission, she has raised two daughters and taken care of her husband. The two of them took up nature photography and planned to publish a book.
After 11 years, Nash knows that Bethany believes in the power of prayer, but right now she’s angry at God.
She slams the armrest and shouts, “It isn’t fair! They said do the surgery and I did. I went through radiation hell. I did everything God told me to do and here I am sick again. It’s all a lie!”
She wails about how her mother prayed when she got cancer, but died. Her friend from church prayed and she died, too. “The women at church prayed with me, and now I’m going to die. All this religion has been a waste of time!”
Bethany’s rant stirs up memories of the doctor’s own losses. It’s hard for him not to feel helpless, but he must remain professional, detached enough to put her needs before his.
“It’s awful, I know,” he says. “I don’t know that I wouldn’t question everything, too, if I were in your shoes.”
He offers her a tissue. She wipes her eyes. They talk about her girls, 10 and 13, around the age Bethany was when her own mother died.
“You grew up to be an accomplished woman despite your mother’s absence,” Nash says. “You took strength in knowing that she loved you. Your girls will make it, too.”
Bethany nods and dabs her eyes. She talks about her husband, Jeff, and their photography book, the shooting trips they took together. She fears he won’t finish the project if she’s not around to nudge him: “You know how he is.”
“You want me to call and remind him?”
A smile breaks out, then a small laugh. “Yeah. It might make him feel less alone.”
Doctor and patient sit quietly together. Then Bethany says, “I want to spend what time I have with Jeff and the kids. I don’t want to go through it again.”
“We can handle the pain without doping you up,” Nash says. Letting go of her hand, he sits back. “This is more than enough for one morning. Can you come back with Jeff so we can draw up a plan? Remember, you are not alone.”
Bethany leans forward to give him a hug. “I’m so glad you’re my doctor,” she says.
The room is dead quiet. For a long moment they hold their embrace, nothing more needing to be said.

Ten moist-eyed medical students then burst into applause for their classmate who is role-playing Dr. Nash and the actress playing Bethany. The scenario is one of many we use at George Washington University medical school in a course I teach called “Practice of Medicine.”
During my medical education in the ’70s, no one ever mentored us in how to handle fraught, terrifying situations like Bethany’s. The vacuum persisted nationwide for decades, especially during the expansion of medical research, the rise of the National Institutes of Health, and the ensuing emphasis on technical interventions and expertise. In 1992, GW became the only medical school in the US with a curriculum that taught young doctors to be “patient-centered”—to respect patients’ beliefs, listen to what patients felt was important, and attend to their existential suffering. The approach sees every ill person as a statistic of one. It stresses dying as a natural part of life—as natural an experience as birth and as meaningful. Today more than 70 percent of medical schools have courses similar to ours.
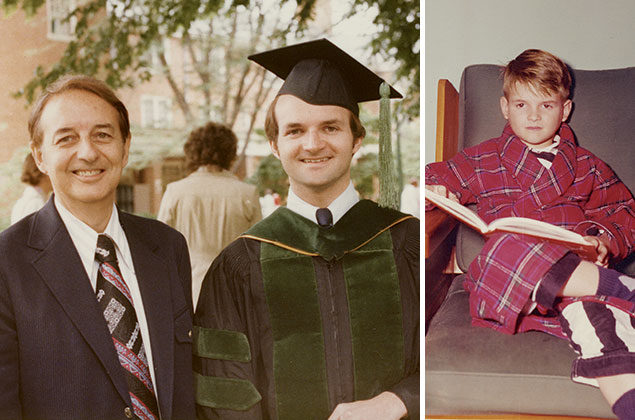
In the ’50s, when my father, also a doctor, took me along on house calls, a majority of people died at home. Today a majority of Americans die alone in hospitals and nursing homes, out of view. There’s something inhumane about this. The blessing of a peaceful death is something too few people experience. The best way to die is in the room of your choice, surrounded by people of your choice, holding the hand of your choice.
Practitioners of my father’s era had to be comfortable with mortality. Families of the dying likewise took it as a fact of life. Generations lived under the same roof, and homes had sickrooms where comings and goings were plain to everybody. Medicine in my father’s day was seen as a calling. It wasn’t uncommon to keep night vigils alongside the sickbed, an activity immortalized in “The Doctor,” Sir Luke Fildes’s famous painting from 1887. A copy of it hung in my father’s office.
His office was attached to our house, as was the custom back then, in the suburbs of Trenton, New Jersey. Patients were constantly around. Emergencies punctuated the dinner hour. Pill samples lay everywhere—the pharmacopoeia of the bread drawer, the basement, the linen closet, the laundry room. When my father took me along on Sunday hospital rounds, we hurried past rows of iron lungs that hulked in the basement entrance off the doctors’ parking lot, a reminder that polio might still take anyone down at any moment.
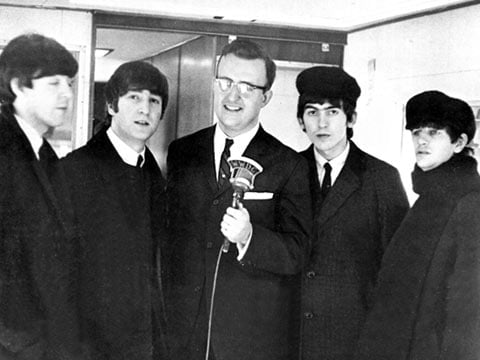
My father did a little bit of everything—delivering babies, setting broken bones, performing surgery, and tending to the quotidian ailments of life. He was also a magician, a hypnotist, a photographer, a swimming coach, and an outdoorsman who threw hunting knives and stalked game with a bow and arrow. Everyone simply called him Doc. By the time I earned my MD at the end of the ’70s, the zeitgeist had changed. No one ever called me Doc.
Dad knew how and when to exploit the placebo effect. His larger-than-life presence made people believe. And in his era, when medicine really couldn’t treat many ailments, he plied the oldest of healing rituals: the laying-on of hands.
Today people can go to the emergency room and be assaulted by a swarm of technology and a bustling staff, yet never once feel the comforting touch of a human hand. This is sad because research tells us that healing occurs within the doctor/patient relationship. Decades after the fact, I heard from people who long ago had been Dad’s patients. “Your father was wonderful,” they said. He didn’t limit himself to asking about their aches and pains. He listened to the whole person. He knew intimate details of their lives.
• • •
One of my father’s patients was Mr. Walter Updike. He owned the bank that held our mortgage, and he looked forward to our house calls. Mr. Updike was a widower and lived alone in one of the biggest houses in town. Three broad steps led up to the wraparound porch, and from there to double glass doors hung with lace curtains. The first time I stepped inside, I noticed the rod at the bottom that held them taut. That’s the kind of thing rich people do, I thought, everything kept in its place.
He and the house smelled old. Bent over, halting, he led us through a parlor with Chinese wallpaper painted with pale blue birds. He offered me ginger snaps on a tray, a gesture I suspected was for my father’s benefit. The two grownups disappeared into another room while I waited on the sofa, taking in the bigness of the house, the crocheted antimacassars on the armrests, the dusty smell of the grand piano. I glanced at the carved archway they had gone through, wondering what mysterious things were happening beyond it.
The next time we visited, my curiosity was rewarded. “Bring the boy in,” Mr. Updike said. “He’s your little apprentice, no?”
“A chip off the old block.”
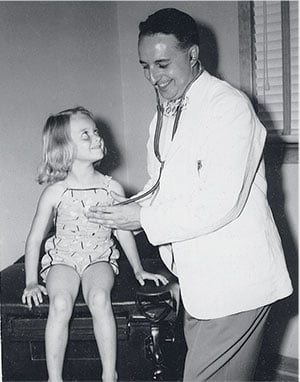
I followed Dad and his black bag into the sickroom. The oblong case was his constant talisman, never far from sight. He set it on the bed, where it fell open along a bottom hinge. From one half he withdrew a stethoscope and sphygmomanometer while Mr. Updike unbuttoned his shirt. Dad listened first to his heart, then to his lungs. He examined the whites of his eyes and then took Mr. Updike’s blood pressure, listening and watching in silence as the gauge needle trickled down.
“It’s up a little. I’m going to give you a shot.”
Mr. Updike turned to me: “That won’t upset you, will it, son?”
No, I told him, though I was glad he was getting the needle instead of me.
From another compartment of the medical bag—in which nestled brown ampoules with such wonderful names as atropine, aminophylline, and morphine—Dad fetched a glass hypodermic. He snapped an ampoule open with a pop and filled the syringe. I watched as the needle pierced Mr. Updike’s hip. The other half of Dad’s medical portmanteau was a traveling dispensary. Neat rows of colorful pills looked out from rows of glass cylinders. He unscrewed one, counted the tablets out and then tipped them into a cardboard pillbox. Still not done, he scribbled on a pad. “You’ll need this prescription, too.”
He wrote his prescriptions in Latin. It infused them with mystery and heightened the art of medicine. My father knew compounding, the formulation of botanical ingredients ground by an apothecary in a mortar and pestle and dissolved in 200-proof alcohol. From thousands in the United States Pharmacopoeia, he knew dozens by heart, ready to be inscribed on his pad in his tight, precise writing. Once I asked him about the enigmatic “Elixir of I, Q, & S.”
“It’s an all-purpose nostrum,” he said. “Iron, quinine, and strychnine—a little of each to lend it some color and make it bitter so patients think it’s doing some good. The alcohol concentration helps the impression.”
• • •
In my father’s era, you were called a medical “intern” because you lived in the hospital. The hours were all day, every day. You did your own lab tests. You looked at your own microscope slides. You sat up with the stricken and enacted the scene in Fildes’s painting.
A generation later, I played that role exactly once. As a student on obstetrics rotation, I was required to sit up through the night with a pregnant woman who was having seizures from eclampsia, a complication involving seizures. My job was to push doses of magnesium sulfate into her IV every time she started to shake. It was impossible to leave her side. Both of us stayed awake through the night. We talked and joked, and she confided her story. A healing relationship was at work, formal but intimate. A generation later, an infusion pump took over my job. How much more comforting must it have been to endure a risky ordeal with someone caring for you at your side than to be left alone with a beeping machine.
I earned my medical degree at age 24 and began my internship on the cancer ward.
As luck would have it, I draw night call on day one. Two fellow rookie interns sign their patients out to me. At midnight, the head nurse summons me to see a man “with trouble breathing.” The chart says he has primary liver cancer with metastases, meaning it has spread to other organs and that his condition is fatal. The nurse shepherds me into his room and closes the door behind us. The lights are down, but I see at once his sunken eyes, his emaciated frame, and his deeply jaundiced skin. He heaves and gasps, each arduous breath spewing blood-tinged froth onto his lips. The pink foam means that his liver can no longer make clotting molecules. He’s drowning in his own blood. His skeletal hand trembles and taps against the bed rail.
The nurse goes to him. “The doctor is here,” she says. She tries to calm him, to no avail.
I lean in close. In the calmest tone I can muster, I ask him what I can do. He turns with effort, his yellow eyes searing into mine. He seems not to comprehend, so I repeat the question and wait, searching for the person still inside the wasted flesh. Suddenly, unexpectedly, he grabs my shirt and pulls me in hard. “Don’t let me die!” he says, spraying me with blood.
I freeze, both of us now terrified, unready for our experience in different ways. The moment is about him yet unavoidably about me, too—the new doctor desperate to do the compassionate thing. The best countermeasure I have is to act calm.
“Get me ten milligrams of diazepam in a syringe,” I tell the nurse, using the generic name for Valium. If he knows I’m sedating him, he’ll only grow more petrified. Inches apart, we regard each other, he like a cornered animal looking for escape while knowing there is none.
The man’s breathing takes heroic effort. Its strident rattling—called in medical terminology “stentorian,” after the powerfully voiced herald in The Iliad—announces impending death. The only tool I have to inspire confidence is emotional calm, my sole purpose at the moment to ease his passing. A peaceful death will signal at least some measure of success.
From the shadows, the nurse hands me the syringe. She mops his brow while I push the viscous yellow medicine into the yellow man’s vein. I take his hand and tell him it will help him breathe. Technically it will, but I purposely invoke the placebo effect, too. Sometimes words have the power to heal. Always they have the power to comfort.
The man settles down, but soon he tugs at my shirt again. “Don’t leave me!” he rasps. His eyes beg. I don’t want to abandon him, but with other calls to answer, I must.
Elsewhere in the hospital, I check on fevers, deal with clogged IVs, write medication orders. Yet my thoughts return to the yellow man’s pleading eyes. Did I let him down?
Hours later, my pager beeps again. It’s the head nurse once more, summoning me back to “pronounce him dead.” He is, obviously, but there are certificates to fill out, a ritual to perform, something else that medical school failed to teach me. The nurse, having seen her share of new physicians, patiently walks me through the process.
Paperwork done, I start to leave. But no, without a word the nurse pulls me to a conference room down the hall. At the threshold, I look to her for explanation.
“The family is waiting to see you,” she says, as if I should have known.
The door closes behind me on a good dozen relatives, all on edge. They look at me expectantly. I panic, thinking of what to say. But then I don’t have to say anything: The family reads my face and laments in unison, wailing and collapsing into one another’s arms. The woman I take to be the deceased’s mother reaches into a purse on the floor and unfurls a rumpled handkerchief. She buries her face in it. Memento mori, the ancient Romans said. Remember that you will die. This scene will be a permanent meditation throughout the rest of my career.
At that moment, my beeper squeals again, freeing me to slip from that unhappy room and exhale. In the hallway, the morning aurora pours through the side windows and catches me by surprise. Then the corridor lights flicker on. It’s the shift change and time for a new day.
Years later, when I was starting out as an attending neurologist at a hospital on Capitol Hill, I was summoned to the emergency room to consult on a lawyer in his late twenties—a man my age—who had had a seizure. The ER attending physician could find no obvious cause. The young attorney, freshly hired as an associate at a white-shoe firm, had been in perfect health until his dramatic convulsion in the Senate chamber.
“What do you remember?” I asked him. “Did you feel odd beforehand in any way?”
He looked up from his stretcher: “No, I was fine. Then I woke up here, very tired. They told me I messed up my pants.” He looked away. “I’m glad I don’t remember that part.”
“These things happen,” I reassured him.
What I didn’t say was that the news was bound to be bad. A first-time seizure in an adult means a brain tumor until proven otherwise. The young man acted cheerful during our examination. He yearned to get back to work. Mentally he was intact—vision and speech normal, no motor weakness or sensory loss. Reflexes were brisk and exaggerated, as expected after a convulsion.
And then I did what would confirm my suspicion: I looked at his retinas with an ophthalmoscope. Both optic nerves were swollen, ghostly white instead of glistening pink as they should have been. I reached for his pulse with my free hand while watching the retinal veins. They should pulsate with each heartbeat, but his lay still. He had florid papilledema, signifying that the pressure inside his skull was quite high. Ominously, it had been that way for some time.
I would have to tell him that the life he’d planned was over—new job, new fiancée, everything he’d imagined stretching out before him about to change. And soon.
It could have been me lying on that stretcher, a twentysomething fresh from graduate school, ambitious, ready to make his mark. It was impossible not to identify with him or to elevate him to special status. From time to time, we doctors do have favorites—patients who pierce the barriers of professional distance and tug at us for reasons beyond logic. When one of them doesn’t make it, the whispers and sidelong glances among the hospital staff reveal just how much the loss makes us grieve.
“I’m afraid it doesn’t look good,” I said to the young lawyer. Everything on the list of possibilities was grim. I assured him he was okay for now, that we had started anticonvulsants. We’d talk specifics once his CT scan was finished.
As expected, his scan did reveal a tumor, but a puzzling one. By definition, a tumor is an extraneous mass that takes up space. One growing within the rigid confines of the skull typically shoves normal structures aside, causing neurological symptoms. But his tumor was as atypical as could be: no distorting mass at all. Instead, it looked as if his brain had been inflated like a balloon, every anatomical structure distended but in correct proportion to the others.
I asked a senior colleague to look at his films. Neither of us had seen anything like it before. With most tumors, one wants to do a biopsy, but in this case nothing suggested a biopsy location or distinguished normal brain from malignancy. His cancer was like crabgrass that had invaded a healthy lawn to form a single, knotted mat. His was the worst kind of condition: a fatal problem that had no solution.
• • •
When I returned to the emergency room, his fiancée was waiting with him. “The tumor has been growing slowly for years,” I said. “That’s why it has remained asymptomatic until now. Eventually it irritated enough neurons to cause a seizure.”
The couple was full of questions and what-ifs. I had relieved some of his intracranial pressure with a spinal tap and started intravenous steroids to retard it from building back up. He was unlikely to have further convulsions. I emphasized that there was no rush, no urgency to “do something,” no matter how alarmed the sudden events made them feel. We had time to weigh options and arrive at a plan together, one that he could accept even if it was imperfect.
The senior partners at his firm thought otherwise. By trade they were fixers used to making things happen. For all the Latin used in their profession, they were ignorant of medicine’s most fundamental adage: Primum non nocere: First do no harm.
They were determined to “save” him no matter what. I had no objection to a third opinion or a transfer of care, but I wanted it done right so that the new physician had all the facts and knew what had transpired so far. But I was no match for the attorneys who wanted things done yesterday.
I was given no time to dictate a discharge summary and arrange for x-ray copies. With no warning, an ambulance showed up and took him away. The resident at the other institution called, predictably irate that the patient had arrived without paperwork. Everything would have to be repeated, and the law partners’ insistence that “everything be done” only inserted false hope. Their efforts would inflict suffering because they would be futile.
Looking back, I wish I’d known how to reassure him better. “Tell me what frightens you,” I could have said. “What do you wish for the most?” If I had been more skilled at the time, I might have defused the race to pile on.
Today at GW we teach our students “perspective taking,” putting themselves in the dying’s shoes, asking, “How would I want to be treated?” What patients want most is to be heard and to feel they’re understood.
The attorney could have spent his remaining months with his family. He was physically fit to travel or engage in whatever he wanted to. He may have needed assistance toward the end, but he could have remained active and involved in the things he cared about most. When the end came, he could have arranged for a peaceful goodbye of his own choosing.
Instead he was subjected to surgery—not surprising given that he’d been sent to a “famous” surgeon. The promise of an “expert” raised expectations that couldn’t possibly be met. Cutting his skull open, subjecting him to anesthesia, and more opened him up to one complication after another.
The more one does, the more that can go wrong. Like trying to turn around an enormous ship, it’s hard to stop the momentum once the system gets going. So today we violate primum non nocere because “we did everything we could” has typically come to mean we’ve done more than we should.
• • •
My students are surprised at how moved they are by the actors. Students begin the course believing the encounters won’t be anything like engaging with a “real” patient. But they discover that they’re emotionally drawn into the scene, even ones far less fraught than bearing bad news. Our actors are versed in improvisation, and although they work from a script, the scene almost always veers off in unexpected directions.
In her post-scene debriefing, the actress playing Bethany gives feedback to the student playing Dr. Nash: “I felt reassured when you said we’d make a plan together to deal with any pain. It was funny, too, when you brought up memories of my daughter wanting to buy me blue hair after it fell out the first time.”
“I wasn’t sure,” says the student playing Nash. “As soon as I said it, I wished I hadn’t. It felt like I was taking your crisis too lightly.”
“No, humor lightened the moment,” the actress says. “I don’t think we could have had that safety valve if we hadn’t already established rapport.”
I ask her what matters most in charged situations like the one we’ve just witnessed.
“When I look in your eyes, I want you to be seeing me,” she tells the group. “I don’t want you to be up in your head where I can see wheels turning.”
Her point is on target. I always see new students ticking off mental checklists, anxious not to miss anything. As they become more skilled, the lists become internalized. Questioning grows flexible and adapts to the moment—it becomes patient-centered.
One student confesses how flustered she felt when Bethany got enraged. The dying can act mad or depressed when what they really are is demoralized, I say. It may feel counterintuitive, but addressing rather than sidestepping existential issues leads to better coping and resiliency at the end.
“How do you say, ‘We’ve done all we can’?”a student asks. “At what point do you try to convince them of reality?”
I go back to our cultural unfamiliarity with death and the end of life. When we rarely observe and participate in it, it’s easy to insist on more procedures, more tests.
“You might lay out how debilitating and expensive an intervention is likely to be when it will have only marginal benefit,” I say. “When you’ve established a therapeutic relationship, it is surprisingly easy to have that discussion. When you can honestly explain that only 8 percent of patients who have CPR survive more than a month, then patients can tell you they’ve had enough. What typically happens, though, is that patients aren’t asked if they want more treatment. It’s forced on them by medical staff or family members who mistakenly urge them to ‘fight.’ ”
I tell the group what the Roman philosopher Seneca said: The fear of death is lessened by meditating on it. In a Botox culture terrified to acknowledge that life is a terminal condition, doctors are situated to speak to these fears. The time to discuss advance directives is when people are well, not at the eleventh hour amid chaos.
One student, quiet until now, shares her astonishment that Bethany thanked the doctor. “I would have felt like I didn’t deserve it, like I had utterly failed by not preventing her cancer from recurring.”
“Are we gods?” I ask. “Should we define success as just keeping patients alive, especially in the face of insurmountable odds?”
I remind them that most clinicians underestimate the healing power of their relationships with patients. For example, pleas for pain pills may be rooted in a patient’s emotional distress. Surprisingly, talking about it can eliminate the need for heavy narcotics. That relief is simple and inexpensive, and the patient is grateful because you’ve given her a sense of control. So perhaps “thank you” is the highest compliment anyone will ever receive.
• • •
And there we end the afternoon. The group is still shaken, and this is our last meeting for the semester. They could use a drink, so we adjourn to a restaurant across the street. As we head out, I think of the challenges my students have ahead. I hope I’ve impressed on them that what distresses the dying most are questions of meaning, hope, and isolation. Better to face such defining human moments having had some practice.
It’s unlikely for now that they’ll have to be the sole bearers of bad news. In their two final years of school, there will be higher-ups for that. But they will observe and, I hope, watch carefully and compassionately. They’ll have to confront the reality that patients do die on them—on the operating table and in the wards. When they take care of patients facing the end of life, I am optimistic they’ll be capable of handling it in a way that brings peace.
I never learned what happened to that frightened young attorney who had a seizure. I wish I could have been there and seen him through to the end. I could have sat silently and listened. I might have focused on caring rather than curing, helped him decide for himself when it was time to stop.
I still picture him looking up at me from that stretcher, frightened and worried.
This article appears in the March 2014 issue of Washingtonian.