Contents
- Spotlight: The Health-Clinic Nurse
- Spotlight: The Covid-Ward Nurse
- Spotlight: The Geriatrics Nurse
- Spotlight: The Triage Nurse
- Spotlight: The Pediatrics Nurse
- Spotlight: The Surgical Nurse
- Spotlight: The Critical-Care Nurse
- Spotlight: The Oncology Nurse
- Spotlight: The Intensive-Care Nurse
- Spotlight: The Operating-Room Nurse
- 50 Exceptional Nurses
- We Asked Our Winners: What Inspired You to Be a Nurse?
- We Asked Our Winners: What Do You Love About Being a Nurse?
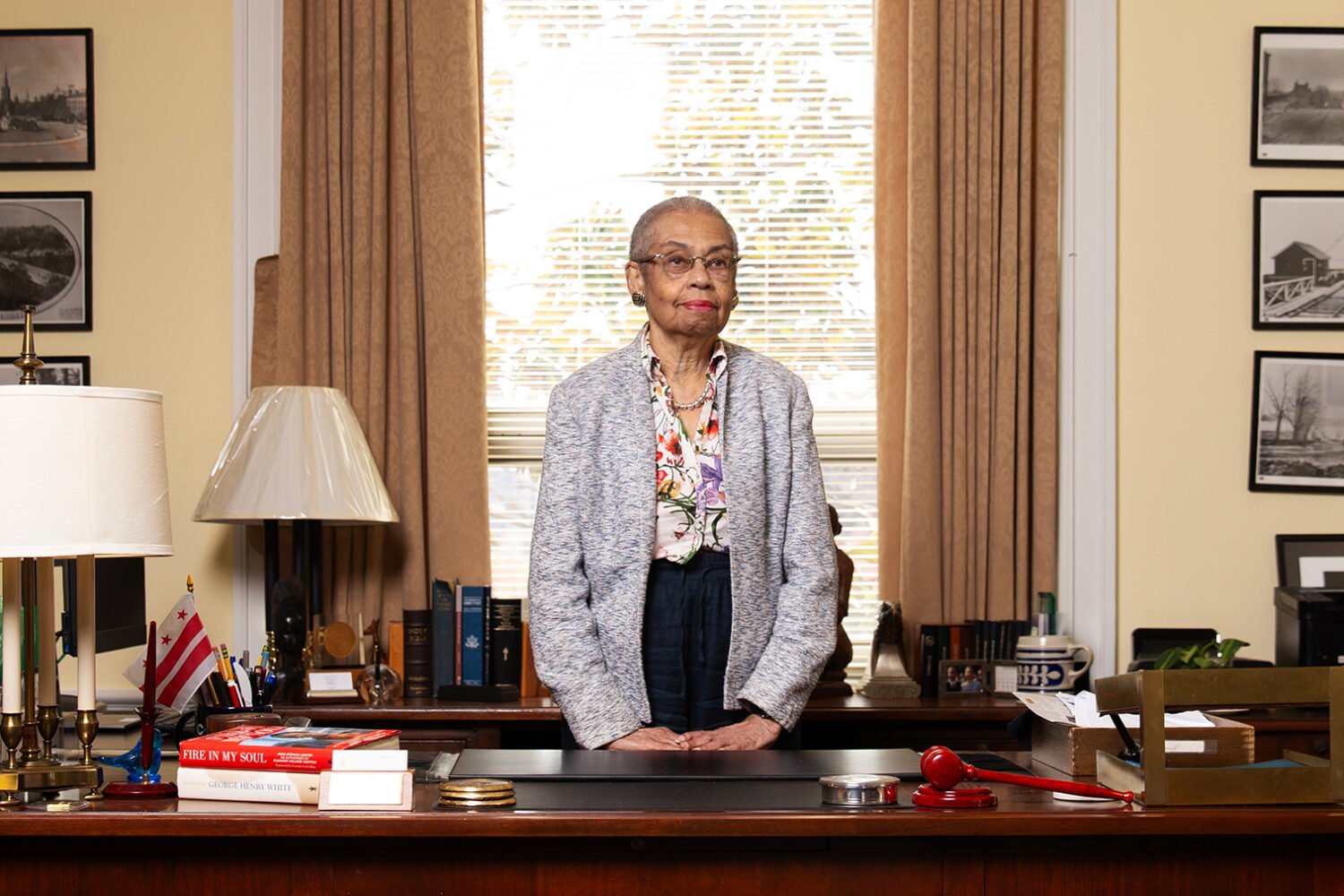
Spotlight: The Health-Clinic Nurse

Michelle Francis
MedStar Georgetown’s School Health Center at Anacostia High
Michelle Francis walked past a student one morning at Anacostia High School—where she works at a clinic run by MedStar Georgetown University Medical Center—then looked back to see him stuff a sleeping bag and duffel into the bushes. Suspecting that the student was homeless, she worked with clinic and school staff to connect him and his family to housing.
“As a nurse, we are trained to be observant,” says Francis, 55, who has been an LPN for 11 years. “I might take a blood pressure and notice cutting on the arm. We had another student, her clothes were dirty. She said her parents didn’t have money for detergent.”
Francis shared with that girl some of her own story—how, when she was growing up in Trinidad in a family of 13, her mother didn’t always have time to launder her school uniform each day. So she explained to the girl how to wash clothes in a sink with a bar of soap.
Francis’s role as a nurse in Southeast DC, where she lives, doesn’t end with her shift: “There was this one instance, I was driving and I observed one of the students with her siblings, and all their possessions were on the side of the street. They had been evicted. I got on the phone, and [she, her two brothers, and her father] were put in a facility that evening. This student was an expectant mother at the time—she was 14 years old.
“We have to look out for each other. For some of our students, there is no one who is looking out for them.”
Back to TopSpotlight: The Covid-Ward Nurse

Rachel Watkins
MedStar Washington Hospital Center
Rachel Watkins will never forget the day last spring when she told her nurses, gathered in a room at Washington Hospital Center, that their 32-bed unit was turning into an all-Covid ward.
“To look at the nurses who had children at home, who were immunocompromised—some cried, some were angry,” recalls Watkins, who hadn’t made the decision but, as nursing director of the unit, had to break the news. “All I could tell anyone was ‘I’m in it with you.’ ”
And she has been, picking up extra shifts on weekends to tend patients. “I don’t ask [my nurses] to do anything I wouldn’t,” says Watkins, 34. “I went in with the first Covid patient who came on the ward.”
Other units transitioned away from Covid care by summer. Hers did not. The result? “My staff,” she says, “was experiencing burnout.”
Watkins had a counselor come to the break room once a week. She planned mood-boosting celebrations such as “Aloha Day,” with steel-drum music and leis. And with another nurse, she adopted a program he’d heard about, Code Lavender. Nurses having a bad day are given a gift bag with a snack, a stress toy, and a purple ribbon to wear so fellow nurses can offer support. Says Watkins: “They’re reminded to take a break, and that your whole team is there to support you.”
The support has helped. Almost a year after the unit was designated all-Covid, the staff was polled as to whether to remain a Covid ward. Watkins says an “overwhelming majority” said yes.
“We all keep coming back because we love working together,” she says, “and we feel we are making a difference.”
Back to TopSpotlight: The Geriatrics Nurse

Rosemary Trejo
Sibley Memorial Hospital
Covid has been particularly devastating to the elderly—including when they’re in the hospital, sick and unable to have loved ones there who might advocate for their care. But at Sibley, some of those patients have Rosemary Trejo to advocate for them.
A geriatrics nurse, Trejo works with patients who are mostly over 80 and in the hospital because of a fall, complications of diabetes, or another issue. She helps shepherd them through treatment and, when necessary, works with them on a post-discharge plan—some may need rehab or other help to live at home again.
“You have to sit with them, which takes longer than a regular patient, and listen,” says Trejo, who asks about their goals and wishes. “Some of them, they repeat the same things over and over. Which tells me it’s important to them.”
Most, she says, want to go home, so she and a team figure out the resources needed to make it happen. “A big part of my role is to be sure that autonomy and dignity is maintained and that their voice is heard,” says Trejo, 59, who has worked at Sibley 32 years.
She became interested in nursing after taking care of her grandmother in her native El Salvador. These days, Trejo cares for her 82-year-old mother, who lives with her.
“Some of these older adults,” she says of her patients, “they had not seen anyone since March, when Covid started. They hadn’t had somebody hold their hand. We do that. We use gloves. I think older adults are used to having someone hold their hand. I never let go.”
Spotlight: The Triage Nurse

Sophia Kim
Gastro Health
When patients call Sophia Kim, they’re sometimes in distress—suffering from a Crohn’s flare-up, possibly, or waiting for a lab report. Kim, 46, does what she can to ease their pain and their mind—including calling on a weekend with test results .
“If I am able, I will look for the results on Saturday to offer them some peace if the results are normal,” she says. “Why wait until Monday to call them? They’re going to be anxious all weekend.”
As a triage nurse, Kim refills prescriptions, checks on patients, and decides when someone needs to see a doctor right away. “I’m the person they call when they’re having symptoms,” she says. “The hardest part is to figure out what is important and what can wait, because to a patient everything is important, even if it’s a Pepcid refill. The reason I do things for patients on weekends and evenings is that even if the issue is not urgent medically, it’s important to them.”
Sometimes it is urgent. “One patient was calling for a simple refill for reflux [treatment]. However, I noticed she did not seem herself,” Kim recalls. “I was able to assess in that five-minute conversation that she needed to go to the ER immediately. When I checked in the next day, she’d had an emergency liver transplant.”
Kim came to nursing at age 35, after being a stay-at-home mom. “With my first child, the birth was traumatic. I had a lot of complications, hemorrhaging and stuff,” she recalls. “The nurses were amazing. I remember feeling a wave of gratitude. I told my husband, ‘I want to be a nurse.’ I wanted to give back to somebody the feeling I had when I was in that place of vulnerability. It took me a while to get there—I had the first baby, then the second. But I never gave up that that was what I wanted to do.”
Back to TopSpotlight: The Pediatrics Nurse

Kim Gerland
Children’s National Hospital
It was late March 2020, and at first Kim Gerland thought her scratchy throat and mild cough were due to allergies. Then came a fever, chills, aches—and a positive Covid test.
For two weeks, she quarantined in her apartment, where she lived with her fiancé, who also contracted Covid. Fortunately, both had mild cases. While she was home, reading and watching TV, Gerland, now 29, learned that researchers were studying whether plasma from survivors could help Covid patients. So when she got the all-clear to go back to her job as a critical-care float nurse at Children’s, she not only volunteered to care for Covid patients, but she looked into donating plasma.
Normally, Gerland would have needed to wait at least a month before donating, to give her body time to recover. But, she says, “due to the severity of Covid last April and having very few people able or willing to donate, I had doctor approval to donate sooner.”
Her rush to help didn’t surprise her coworkers, who call her not only an “exceptional nurse” but a “team player.”
Donating plasma is like giving blood, except that the needle is bigger and stayed in her arm for an hour. The second time Gerland went to donate, she learned that her iron levels were almost too low. Afterward, she was very fatigued. She had wanted to keep giving plasma but stopped because of her iron deficiency.
“While I wanted to donate again,” she says, “I did feel a sense of relief knowing that once people started to learn more about it, the blood-donation center had more people going in and donating.”
Back to TopSpotlight: The Surgical Nurse

Mansoureh Akbari
Kaiser Permanente
Kaiser Permanente’s Kensington clinic was experiencing a shortage of nurses certified in wound care, meaning that patients who had had reconstructive plastic surgery sometimes couldn’t get wounds tended on a particular day. On her own time, Mansoureh Akbari decided to study for a wound-care certification, going on to earn it in about three months.
“I thought, ‘If I can get the certification, I can be more helpful,’ ” says Akbari, 45, who grew up in Iran.
That was in 2019. Then in 2020, Akbari earned another certification, in ostomy care, when the clinic was shorthanded there. She did this, says her supervisor, Kevin Estrada, despite having an increased workload after another nurse was reassigned to assist with Covid patients. Akbari had to run both the general-surgery and plastic surgery nursing departments, supervising patient flow, directing clinical staff, assisting with procedures, and responding to patients who reached out with questions and concerns.
She says she particularly connects with breast-cancer patients: “I think one thing that has helped me a lot in my work is that I had breast cancer more than three years ago. Sometimes they come and they cry in the beginning, and when I tell my story, some are surprised to see me working and healthy and happy. I think that helps me and them. I feel like I am being helpful.”
Spotlight: The Critical-Care Nurse

Priscilla Thompson
Adventist HealthCare White Oak Medical Center
When someone having a stroke or heart attack is rushed into White Oak Medical Center in Silver Spring, Priscilla Thompson, a critical-care crisis nurse for 29 years, may be the one who reassures the often confused, frightened patient.
She might hold the person’s hand, look him or her in the face, and say everything is going to be okay.
“I find that people fail to speak to the patient,” says Thompson, 59. “They still hear you. They still see you. There is a fear [in patients] of what’s going on. The only thing I have to offer them besides clinical knowledge is hope to hold on and let them know we will do everything we can.”
The masks and respirators required during the pandemic have made it harder for a patient to hear what Thompson is saying.
“All you have is your eyes,” she says. “Later, I’ll follow up with them in the ICU and they’ll see my eyes and say, ‘I remember you. You are the only one who talked to me.’ ”
Back to TopSpotlight: The Oncology Nurse

Lorraine Waltz
Virginia Hospital Center
If Lorraine Waltz senses a cancer patient is struggling, she might ask if the person likes poetry, then reach into her pocket for a favorite verse.
“One of my go-tos is Emily Dickinson’s ‘Hope Is the Thing With Feathers,’ ” she says, breaking into the first verse:
Hope is the thing with feathers
That perches in the soul,
And sings the tune without the words,
And never stops at all . . . .
“Dying is hard,” says Waltz, 55, of Virginia Hospital Center in Arlington. “When a patient and I share an interest in literature, I ask permission to bring them a poem a day as a diversion. For people who want to fight, I might give them Dylan Thomas’s ‘Do Not Go Gentle Into That Good Night.’ For people starting radiation, I pull out ‘The Radiation Waiting Room’ [by Susan Herron Sibbet]. My favorite pocket poem is Stanley Kunitz’s ‘The Layers.’ ”
Waltz, who has attended summer writing programs at Sarah Lawrence College, journals and writes poetry—often about what she has witnessed that day. “That’s the reason I’ve been able to survive as an oncology nurse as long as I have,” she says.
The patients also keep her going. As patient-care director in oncology, she visits each of what could be 21 patients every day. That can take up to two hours.
When a leukemia patient was cut off from loved ones due to Covid, Waltz arranged a family “gathering” separated by glass. For a young woman whose last wish was to marry her longtime partner, Waltz put on a wedding. The bride died later that night.
“We might be with a patient a month, especially leukemia patients,” Waltz says. “We get to know them in a way that’s really intimate. It’s a privilege. It really is. There are all the technical tasks of nursing—putting in IVs and hanging blood. But it’s great to handle that spiritual part.”
Back to TopSpotlight: The Intensive-Care Nurse

Davon Foggo-Adams
George Washington University Hospital
Davon Foggo-Adams recalls his first coronavirus patient, in March 2020. “Initially, I was apprehensive about taking care of a Covid patient when we didn’t know much about the disease,” he admits. “But once I put on my PPE and stood at the door of that isolation room, that patient’s health was the only thing I was thinking about.”
His mother, a nurse in Bermuda, where he was born and raised, worried for him. “Almost every day, my mom would reach out: ‘Are you okay? Do you have a fever?’ ”
Early in the pandemic, Foggo-Adams had a Covid patient who was declining quickly, and—before this became more common—he arranged a FaceTime call with the person’s loved ones so they could say goodbye. Foggo-Adams stayed by the patient’s side, holding his hand during his final moments.
“In the past year, I’ve seen countless patients die,” says Foggo-Adams, 31, who has been a nurse for seven years and also teaches nursing at GW. “Sometimes we saw two or three die in a day. Working in the ICU, we’re used to seeing patients die, but three in a day—that’s abnormal. I always say nursing is a calling. You don’t get into nursing if it’s not something you want to do.”
Spotlight: The Operating-Room Nurse

Laila Bailey
Inova Fairfax Hospital
A surgeon in the middle of an operation can’t always know exactly how surgery will go. Complications can arise. The doctor may suddenly need a different suture or piece of equipment.
At Inova Fairfax, Laila Bailey, the service leader in the ORs for both urology and pediatric general surgery, tries to foresee every possible need. “Her ability to anticipate what may occur in the OR is amazing,” says urologic oncologist Inger Rosner.
Says Bailey, 60, who has been at Inova Fairfax almost 36 years: “It’s my job to make their job easier.” If that means taking a call at 11:30 at night or while on vacation, she does it gladly.
She also tries to make surgery easier for patients.“When I meet a patient in the pre-op area, I try to put them at ease as much as possible” says Bailey, whose mother was an OR nurse. “I had surgery two years ago—I had breast cancer—and it’s a humbling experience to be a patient. You have to give up control to other people at a very scary time. In the OR, I help [patients] onto the bed. I let them know what’s going on. I hold their hand as they fall asleep. I want them to know that they are not alone.”
Back to Top50 Exceptional Nurses
Nurses who go above and beyond every day for their patients and colleagues
Mansoureh Akbari
Reconstructive and General Surgery
Kaiser Permanente Kensington
Minna Manalo Bacarra
Nurse Practitioner, Breast Surgery
Inova Schar Cancer Institute
Laila Bailey
Urology and Pediatric Surgery
Inova Fairfax Hospital
Elissa Barpal
Internal Medicine
GW Medical Faculty Associates
Dawn Beauchamp
Nursing Director, ICU
MedStar Washington Hospital Center
Jennifer Bliven
School Nurse
Our Lady of Good Counsel
Melissa Borofsky
Otorhinolaryngology Surgery
GW Medical Faculty Associates
Meghan Bozzelli
Patient Care Director, Emergency Department
Virginia Hospital Center
Caitlin Brown
Clinical Team Lead
Potomac Pediatrics
Mariana A. Capati
Magnet Nurse Practice Leader
Kaiser Permanente
May Capulong
Internal Medicine
Kaiser Permanente Springfield
Christine Chaney
Cardiothoracic/Trauma/Medical ICU
George Washington University Hospital
Claire Dejou
Nurse Manager, Neurosciences ICU
MedStar Georgetown University Hospital
Melody F. Dickerson
Senior Vice President and Chief Nursing Officer
Virginia Hospital Center
Christy Drake-Mauney
Ambulatory Nurse Coordinator
MedStar Washington Hospital Center
Lisa Dreyfuss
Pediatric GI/Aerodigestive
MedStar Georgetown University Hospital
Simone Duru
Orthopedic Surgery
George Washington University Hospital
Mourine Evans
Director, Conway Nursing Pathfinder Program
Children’s National Hospital
Sharon Ferguson
Post-Anesthesia Care
Suburban Hospital
Davon Foggo-Adams
ICU
George Washington University Hospital
Michelle Francis
Pediatrics
School Health Center at Anacostia High (MedStar)
Susan Frank
Oncology Patient Navigator
Inova Schar Cancer Institute
Kim Gerland
Critical Care
Children’s National Hospital
Debbie Jenkins
Nurse Manager, Medical/Surgical
Sibley Memorial Hospital
Ellen Katz
General Medicine
Inova Fairfax Family Practice
Lauren Keane
Nurse Manager, Endoscopy
Gastro Health
Ken Kilemi
Nurse Manager, Inpatient Oncology
Sibley Memorial Hospital
Sophia Kim
Triage
Gastro Health
Megan Kline
Acute Care
Holy Cross Germantown Hospital
Amanda Loop
Nurse Manager
Providence Urgent Care Center
Ann Marie Matlock
Service Chief/Captain, United States Public Health Service
National Institutes of Health Clinical Center
Kimberly Miller
Nurse Practitioner, Plastic and Reconstructive Surgery
MedStar Georgetown University Hospital
Craig Moseley
Resource/Emergency Response Team
Reston Hospital Center
Loan Nguyen
Medical Stroke Unit
Virginia Hospital Center
Cindy Notobartolo
Administrative Director, ED/Trauma, Safety, Security and Employee Health Services
Suburban Hospital
Julen Pamphille
Infectious Disease Clinic
Kaiser Permanente Capitol Hill Medical Center
Sally Parris
Director, Occupational Health
Virginia Hospital Center
Captain Tyeara Phifer
Critical Care
Walter Reed National Military Medical Center
Ashley Reeves
Pediatric Procedural Sedation Unit
MedStar Georgetown University Hospital
Jeanne R. Ricks
Executive Director, Ambulatory Nursing
Children’s National Hospital
Mary Santerre
Manager, Occupational Health
Children’s National Hospital
Donna Spurlock
Internal Medicine
Loudoun Internal Medicine Associates
Ruth Sullivan
Patient Care Nurse Navigator
Inova Schar Cancer Institute
Mariela Tellez
Surgical Services
Sentara Northern Virginia Medical Center
Priscilla Thompson
Critical Care Crisis
Adventist HealthCare White Oak Medical Center
Rosemary Trejo
Geriatrics
Sibley Memorial Hospital
Lorraine Waltz
Patient Care Director, Oncology
Virginia Hospital Center
Rachel Watkins
Nursing Director, Covid Unit
MedStar Washington Hospital Center
Connie Wisnaes
Obstetrics/Gynecology
Kaiser Permanente Burke
Michelle Vassallo
Vice President of Nursing, Clinical Platforms
Inova Health System
We Asked Our Winners: What Inspired You to Be a Nurse?
“In 1978, I was born by emergency cesarean section with double-collapsed lungs from meconium aspiration. My Apgar scores and initial 24 hours of life did not predict a successful outcome. However, those nurses and doctors worked miracles, and after 14 days I came home—completely recovered. I wanted to be a nurse who delivered miracles.”
Jennifer Bliven, Our Lady of Good Counsel School (Vienna)
“I wanted to become a nurse since I was five. My grandma was a diabetic, and I remember stealing her syringes from the trash and filling them with fluids and injecting my dolls and playing nurse.”
Christine Chaney, George Washington University Hospital
“When I was six, my grandfather had to give himself insulin every morning. I would run down and watch. The whole thing intrigued me.”
Ellen Katz, Inova Fairfax Family Practice
“The summer before my senior year of high school, I was in a bad car accident. I was T-boned. I had a lacerated spleen, a collapsed lung, a broken pelvis. I was in the hospital about a week. I fell in love with the nurses. They would sit at my bedside and hold my hand, talk me through everything. After that, I thought, ‘I’m going to be a nurse.’ ”
Kimberly Miller, MedStar Georgetown
“My mom’s a nurse. The minute I graduated, I applied to where my mom worked and got my first job. I have a picture of my mom and me in scrubs, working together in the ER.”
Cindy Notobartolo, Suburban Hospital
“I was inspired to become a nurse when I was 14. My younger brother Teddy became acutely ill. He spent months at Children’s Hospital of Philadelphia. To this day, I have fond memories of watching the nurses soothe his fears.”
Sally Parris, Virginia Hospital Center
Back to TopWe Asked Our Winners: What Do You Love About Being a Nurse?
“Being with someone at perhaps the worst time in their life and helping to make it just a little better.”
Dawn Beauchamp, MedStar Washington Hospital Center
“When people are sick and cannot speak for themselves, I become their proxy. I am the outspoken nurse ensuring that all of their needs are heard and met.”
Simone Duru, George Washington University Hospital
“There’s a connection a nurse makes with a patient that is indescribable. They trust you with their life, and that is something sacred I don’t ever take for granted.”
Melody F. Dickerson, Virginia Hospital Center
“Nursing is focused on care versus cure. It doesn’t mean I don’t want patients to be cured. But we’re not just fixing their runny nose—it’s taking care of their entire being. And in pediatrics, it’s often taking care of the entire family.”
Caitlin Brown, Potomac Pediatrics
“I wear something silly on my head every Friday. I have 150 to 200 silly hats. I just like to make people smile.”
Donna Spurlock, Loudoun Internal Medicine Associates
“The thing I love is connecting with patients. This was certainly validated during this pandemic. With all of the restrictions, I often found myself playing nurse, daughter, friend, comforter, advocate, or whatever I needed to be to help patients get through the hard times.”
Captain Tyeara Phifer, Walter Reed National Military Medical Center