Triple-negative breast cancers can be challenging to treat, but treatment can manage them in many cases. Bonnie Sun, M.D., a Johns Hopkins surgeon specializing in breast cancer treatment, explains triple-negative breast cancer, the outlook for patients and reasons for hope.

What does “triple negative” mean in terms of breast cancer?
Normal breast cells have receptors that respond to hormones such as estrogen and progesterone, which allows them to grow and regress in response to the hormone level. Hormone receptors may or may not be present in breast cancer. About two-thirds of breast cancers are “positive” and contain these receptors like normal breast cells do. These are less aggressive cancers that are less likely to need chemo and are often treated with hormone therapy and surgery. Radiation may or may not be needed.
HER2/neu (hormone epidermal growth factor receptor 2), is a protein molecule that has a role in cell proliferation in normal cells. In some breast cancers, this protein is overly produced or “positive.” For HER2-positive tumors, there is a specific medication that targets this protein.
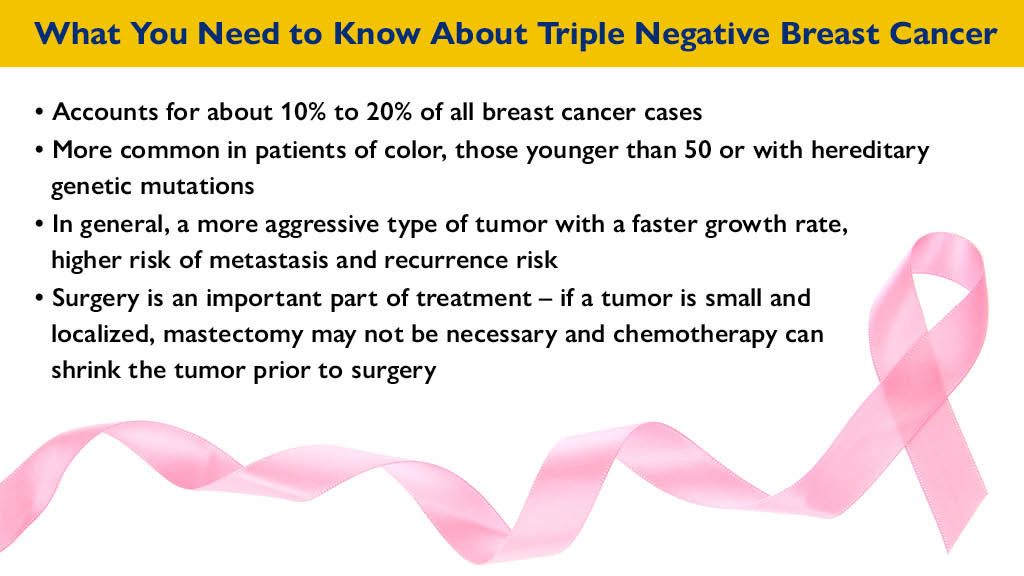
Triple-negative breast cancers are not positive for estrogen receptors, progesterone receptors or HER2 protein. “Since these targets (hormone receptors and HER2) are absent in triple-negative breast cancer, chemotherapy is needed,” Sun says. “Triple-negative breast cancer is often very sensitive to chemotherapy, which, despite the side effects, is an effective treatment that can save lives. Because this is an aggressive cancer, treatment is aggressive also. But there are several ways we can address it.”
What is the treatment for triple-negative breast cancer?
“Chemotherapy is almost always called for,” Sun says. “Chemo can downstage tumors (shrink them or make them less aggressive).” While Sun says chemotherapy for triple-negative breast cancer can be intense, she adds that regimen can be tailored to the individual and adjusted for older or frailer patients.
“In those cases where we get complete response, we know we gave you the right medicine and your prognosis is good,” Sun says.
“Surgery for triple-negative breast cancer does not always have to be a mastectomy,” Sun says. “Effective chemotherapy done first opens the possibility of less-invasive surgical options that are less of an ordeal for the patient. If the tumor is small enough after chemo, outpatient procedures or a lumpectomy may be possible.”
Surgical samples of the cancerous tissues taken during surgery can provide more information on the cancer and how it is behaving so chemotherapy can be tailored accordingly.
Radiation therapy involves beams of radiation to destroy cancer cells, using various techniques to prevent damage to healthy surrounding tissue.
Medical treatments are being tested on triple-negative breast tumors in clinical trials.
- Newer medicines called poly (ADP-ribose) polymerase inhibitors or PARP inhibitors can destroy cancer cells and are now FDA-approved to treat triple-negative breast cancer.
- Immunotherapy helps your body see the malignant cells as harmful invaders so your immune system can fight the cancer. Though not usually a first-line treatment for this type of cancer, immunotherapy can help certain patients in very specific situations, Sun notes.
“Immunotherapy and PARP inhibitors are very exciting and there’s lots of research going on, including here at Johns Hopkins,” Sun says.
What is the prognosis for triple-negative breast cancer?
A good treatment result depends on several factors. “Chemotherapy is what can really make a difference in the outcome. The size of the invasive part of the tumor, and the number of involved lymph nodes can also greatly influence your prognosis,” Sun says, but adds that if the cancer has spread (metastasized), the prognosis is less certain.
“There is hope, even with this serious diagnosis, and staying optimistic is essential. It can be stressful and scary to go through chemo, but positive thinking can make a difference. You have to believe that it’s doing you good, and for most people, it does.”
Learn more: hopkinscancerdc.org


