Something Happened and We Don’t Know Why
There’s a light breeze over Rehoboth Beach as five-year-old Elizabeth Polanin takes her dad’s hand and walks toward the ocean. “That is one big pool, isn’t it, baby?” her father says.
The water comes close, so Elizabeth steps back. She smiles and shakes a hand in the air, a sign she’s excited, then covers her ears as a wave crashes—like many children with autism, she’s sensitive to sounds.
When the water recedes, Elizabeth walks toward it again, making high-pitched sounds and rubbing her hand against the back of her head. “You’re getting brave now!” her father says.
Water is one of Elizabeth’s favorite things. She once took ten baths in a day. She’ll happily sit in her inflatable pool at home in Greenbelt and watch a toy spin in the water.
Her twin brother, William, likes water too. He used to leave the faucet on for hours and watch it flow.
When Elizabeth comes back from the ocean, she jumps into her mother’s lap, accidentally hitting her.
“Don’t hit people,” William tells his sister. “Don’t hurt your William. Don’t hurt your peoples. Don’t hit your peoples.”
Elizabeth doesn’t respond to her brother. She used to when they were babies, but now she hardly talks at all.
“These children were normal that first year and a half, as normal as two babies could be,” says Joe, her father. “Something happened to them, and we don’t know why.”
Autism is a spectrum disorder—children who have it exhibit a wide range of behaviors. William talks; Elizabeth rarely does. He sleeps in a bed; she sleeps in a crib. He’s learning to write letters and numbers; she’s learning “come here” and “stop.”
The National Institute of Mental Health defines autism as a developmental disorder characterized by an impairment in thinking, feeling, language, and the ability to relate to others. William and Elizabeth fall on ends of the spectrum. He’s “high-functioning,” and she’s “low-functioning.”
According to the Autism Society of America, autism is the nation’s fastest-growing developmental disability. One in 166 children has an autism-spectrum disorder—four times as many boys as girls—and about 40 percent don’t speak.
In Prince George’s County, where William and Elizabeth attend school, more than 800 students fall on the autism spectrum; about 250 did in 1999. Montgomery County has 943 students with an autism-spectrum disorder, and 28 classes exclusively for children with autism. Fairfax County has 1,188 students receiving autism services, up nearly 50 percent from five years ago. Arlington had 87 students on the spectrum in 2001 and has almost twice that now. Loudoun has 450. Alexandria has 63. (DC Public Schools did not provide figures.)
Researchers don’t know what causes the brain abnormalities that lead to autism. Evidence supports both genetic and environmental factors. Nobody knows why the numbers seem to be rising. Some think the high rates have always been there but children now are more accurately diagnosed. Others argue there’s an epidemic.
Neurodevelopmental pediatrician Chuck Conlon, who treats William and Elizabeth, says: “I know very few people, if anybody, who don’t have some connection to someone with autism.”
When Julie Polanin gave birth to two healthy babies in June 2001, she and Joe didn’t give autism a thought.
Julie tried for three years to have children. She was 35 when she found out she had a benign fibroid tumor in her uterus. If she had it removed, doctors told her, the procedure would turn into a hysterectomy, and she wouldn’t be able to have a child.
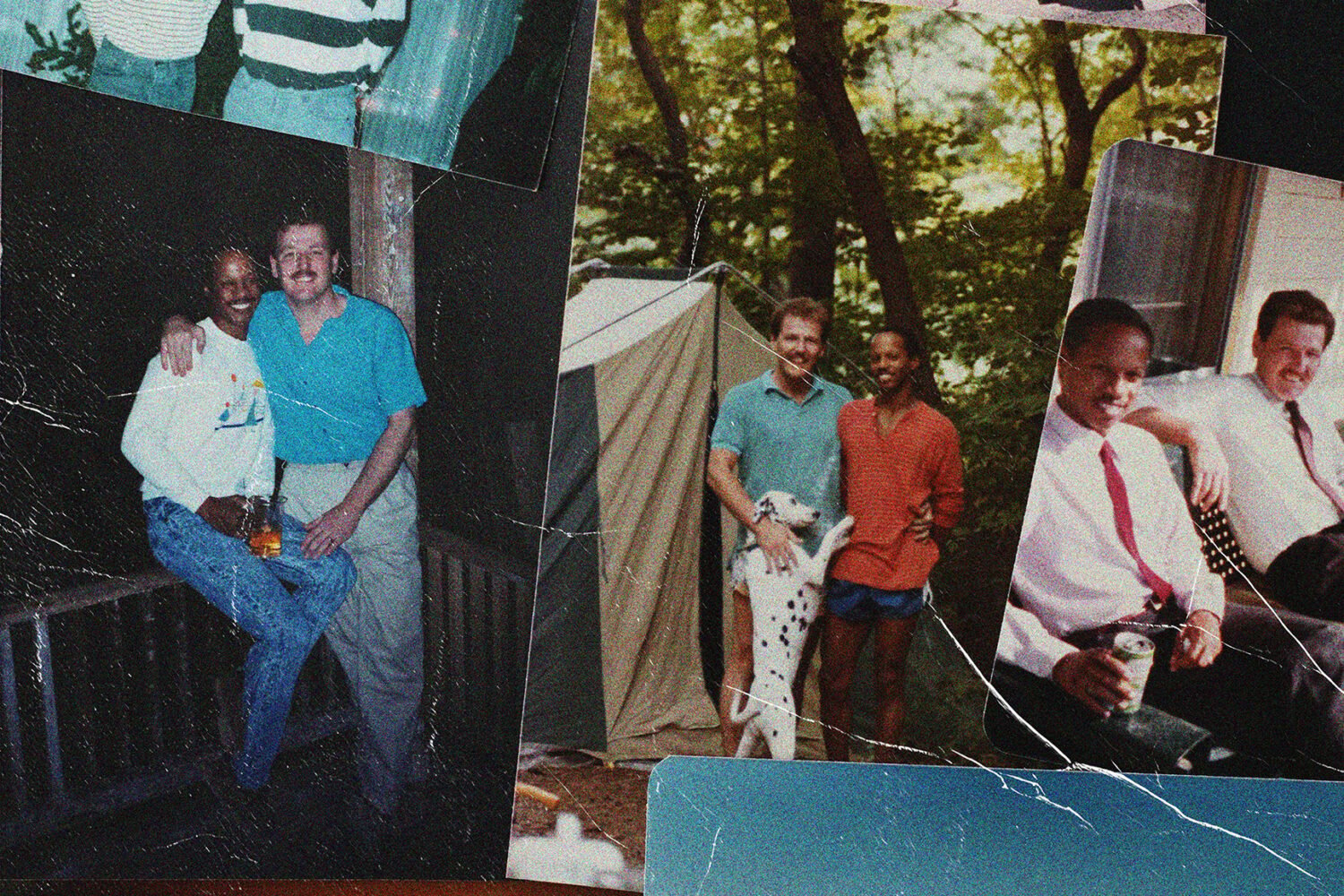
Julie had finally found the man she wanted to have children with. She’d met Joe Polanin in 1989 while they were working at a Silver Spring nursing home. He was office manager; she coordinated social services. He had custody of his two older sons. Joe and Julie both loved music. She fell for his quirky sense of humor. They married in 1995.
Joe knew it was late to become a father again—he’s now 60—but he knew how much fun kids could be and how much a child meant to Julie.
They found a doctor who could perform the surgery without removing Julie’s uterus. She miscarried two years later in 1999, but doctors were still optimistic.
Julie stayed away from alcohol and caffeine. She avoided fish because she worried about the effects of mercury. She drank bottled water.
In October 2000, she was pregnant again. A sonogram showed twins. Julie was ecstatic.
Six months into her pregnancy, Julie went into preterm labor. Doctors put her on bed rest for three months. Every day, she read about how the babies were growing inside her.
At 38, Julie knew she was at higher risk for Down syndrome. She and Joe agreed to have amniocentesis.
A nurse called soon after and told her, “Your babies are perfect.”
It’s June 2006, and the twins are turning five. A photo on their birthday cake shows them as infants, sitting in the green felt pouches they were in at Halloween. “Two peas in a pod,” their parents called them. The icing on the cake reads my how you’ve grown.
William sits in a hammock, wearing a Spider-Man T-shirt, playing with a toy that churns out bubbles. Elizabeth wanders in and out of the house, unaware she’s turning five today.
The Polanins’ backyard is a private playground. William makes racetracks from sticks and mulch for his toy cars. He rides a tricycle into a small tree, repeatedly saying, “Oops—he crashed.” He looks for trolls hiding among the trees.
Elizabeth often sits in the pool chewing on a toy, or swings so fast that the swing set shakes. She stands on her tire swing and twirls around.
There’s one other child at the party; most guests are Julie and Joe’s friends. William and Elizabeth usually play alone. Neighborhood kids don’t come over—Julie thinks their parents aren’t comfortable letting them play at her house.
“It’s time to cut the cake!” Joe yells.
“Not yet,” William says. He walks to the back door, his hands over his ears. “Let’s go in the house.” He watches from inside the doorway while the others stand near the cake in the backyard and his mom blows out the candles.
Julie and Joe hoped William and Elizabeth would be starting kindergarten soon. Joe would be retiring in a few years from his job as accounts specialist at Adventist Healthcare, so he would be there to greet them after school.
He looked forward to age five as a turning point, as it had been with his older sons. That’s when a parent’s job got easier.
When Dr. Chuck Conlon started his pediatric training at Bethesda’s National Naval Medical Center in 1979, the medical community was just beginning to understand autism. A young patient at the center, who exhibited repetitive behaviors and language that was unclear and disconnected, was diagnosed with “childhood schizophrenia.” Doctors didn’t know what they were seeing.
Autism had been identified in the 1940s by Leo Kanner, a physician at Johns Hopkins Hospital. He studied 11 children who showed signs of social isolation, limited speech, and lack of emotional attachment, and he introduced the label “early infantile autism.” But the term wasn’t widely accepted until the 1980s.
Around the same time Kanner identified autism, an Austrian named Hans Asperger observed a behavior pattern in boys that included normal intelligence and language development, and difficulty adapting to a social environment. It was named Asperger’s syndrome. Both autism and Asperger’s fall under the category of pervasive developmental disorder.
People with Asperger’s also exhibit a range of behaviors, including fixation with a single topic, difficulty understanding abstract concepts, repetitive rituals, socially inappropriate behavior, and lack of coordination. Many such children have a high level of vocabulary. They’re often described as “eccentric.”
In some children with autism, the behavioral signs are subtle; in others, they’re easy to see. “People think about the worst-case scenario,” Dr. Conlon says. “No language, doesn’t interact, never makes eye contact. That’s the rarity these days.”
As babies, William and Elizabeth liked to steal each other’s bottles and toys. Elizabeth laughed at her brother when he rubbed food all over his face. They sat next to each other and played. When Elizabeth was sad, William cried.
Both crawled by six months—earlier than many. Elizabeth liked looking at tags on pillows. She’s going to be a reader, Julie thought.
Julie and Joe took the kids on a winter trip to Rehoboth Beach, where William and Elizabeth enjoyed the hotel’s indoor pool and Elizabeth tasted her first Krispy Kreme doughnut.
By ten months, Elizabeth had started saying “Daddy.” William knew “Mama,” then “cool” and “hot.” Elizabeth walked at a year, a month later than her brother. Around that time her eyes changed from blue to gray.
Fifty people came to celebrate their first birthday. Elizabeth and William scooted around in carts. William said “ooh” and “aah” after every gift was opened.
Elizabeth fell asleep eating cake, and Julie took pictures of her covered in chocolate.
When Julie saw a Washington Post article this September about a study linking autism in children to the age of the father, she sent Joe an instant message.
The study showed that the chances of having a child with autism are five times greater for a father in his forties than for a father in his twenties, and nine times higher for a father in his fifties.
“Did you read it?” she asked.
“Yup, I read it,” he said.
She dropped the subject. She didn’t want Joe to think she was blaming him.
Julie had always thought it was unfair that older women had to worry about having children but older men didn’t. She’d never considered Joe’s age an issue, and doctors hadn’t mentioned it.
“You want children so badly, and time clicks away,” Julie says. “You don’t really sit down and think that these things can happen.”
Joe didn’t get upset when he heard about the age study. He’d heard lots of explanations for autism: The mercury once contained in the measles, mumps, and rubella (MMR) vaccination; lead levels in the air from the cars driven while he was growing up; mercury exposure from coal-burning power plants.
“When people look at the Strom Thurmond and Hugh Hefner types having healthy children, they think it must be okay for guys,” Joe says. “That may not be true.”
Autism researchers continue to focus on brain structure. A study by the University of California at Davis’s MIND Institute—the acronym stands for Medical Investigation of Neurodevelopmental Disorders—showed that males with autism have fewer neurons in the amygdala, a part of the brain associated with emotion and memory. Autism has also been linked to rapid brain growth during infancy.
A study released in June by the Yale University School of Medicine found differences in the placentas of children who fall on the autism spectrum, prompting the headline test could spot autism at birth.
Julie still believes her kids’ problems are connected to the MMR vaccine they had when they were a year old. Even if genetics are a factor, she says, the mercury in that vaccine and others since probably triggered the autism: “Why would anyone put a known neurotoxin in someone’s body?”
Thimerosal, the mercury-based preservative used in the vaccine, has been the subject of debate for a decade. Many large-scale studies have disproved a link between Thimerosal and autism. Last April, nearly 1,000 people gathered in DC for the Mercury Generation March, lobbying for more research. The FDA reports that Thimerosal has been virtually removed from almost all vaccines for kids under seven.
Joe isn’t sure why his children have autism. Early on, he blamed the vaccine. Now he wonders if it’s a combination of factors, including genes. He has no regrets.
“There’s no undoing something you did yesterday,” he says. “You can’t stop living because of all the risks involved.”
In December 2002, when she was 18 months old, Elizabeth stopped responding when Julie called her name. Elizabeth liked looking out the window. She liked watching wheels spin.
Julie didn’t know much about autism: She thought children who had it banged their heads against walls and bit people.
Soon after Christmas, Elizabeth stopped coming to her parents for hugs. She was more interested in watching things in motion than she was in people. She seemed confused, like the Alzheimer’s patients Julie helped in the nursing home. William was playing with wooden trains and putting puzzles together.
That May, the family took a two-week trip to Illinois for the wedding of one of Joe’s sons. In the months before they left, Elizabeth could sing along with “Wheels on the Bus.” She could dance like a ballerina.
On the trip, she cried a lot. She stopped eating with a spoon. She clenched her hands together and rolled her eyes. She stopped saying the words she’d learned, like “ball” and “good girl.”
Julie asked other parents if their children had ever lost their language. “Yes,” one mother told her, “my son just decided he wasn’t going to talk for a while, then started again.”
“All right!” Julie said. “Did you hear that, Joe?”
She sang “The Ants Go Marching,” hoping Elizabeth would sing the “boom, boom, boom” in the refrain as she always did. Her daughter stared at her.
When Julie looks back at photographs of William and Elizabeth, the professional shots where they’re sitting together, she can see their transformation.
“The first year, they looked right at the camera,” she says. “The second year, she’s looking over to the side, and he’s looking straight on. The third year, we couldn’t get either one of them to look.”
About 30 percent of children with autism go through a regression, losing some of the skills they’ve developed.
“In some children with autism, development looks relatively okay but then begins to derail,” says Dr. Rebecca Landa, director of the Center for Autism and Related Disorders at Baltimore’s Kennedy Krieger Institute. “For some children there are telltale clues at 14 months that help us predict whether the child will have an autism outcome. But it’s hard to predict the kids who are going to have a regression.”
Until recently, some members of the medical community weren’t convinced that children regressed. They argued that parents must have missed the signs.
University of Washington researchers studied 56 home videos of children’s first- and second-birthday parties. Among the findings: They saw two-year-olds with symptoms that hadn’t been visible a year earlier. At 12 months, children diagnosed with regressive autism used complex babbling and words more often than did those with early-onset autism.
“We can screen for autism early, but we have to screen at least until the child is three,” says Dr. Landa. “We don’t want to just screen a child one time around their first birthday and say to a parent, ‘You have a clean slate. Your child will never have autism.’ We’re just not there yet.”
Julie looked for reasons why Elizabeth couldn’t have autism: Speech comes more slowly for twins. Maybe she and William had their own language. Elizabeth had been born with torticollis: Her head was turned in the womb, causing the muscle on one side of her neck to be shorter than the other—and one side of her head was flatter than the other. Maybe that was the problem.
Julie called friends and relatives: “You don’t think this could be autism, do you?”
Elizabeth continued to stand in place and roll her eyes, making Julie wonder if she was having seizures. Julie and Joe took Elizabeth to a neurologist at Children’s Hospital in July 2003, when she was two. Joe waited in the hallway with William.
“Is it okay if I let her run?” Julie asked. Elizabeth ran toward the opposite end of the room, where the doctor was sitting, but didn’t look at him. She stopped and stood still, excitedly clenching her fists, then holding them in place.
The doctor asked Julie, “What’s your take on this?”
“I think it could be autism,” she said, “and I’m hoping it’s not.”
“You’re right,” he said. “It is. I don’t have to do any real tests with her.”
Julie felt sick.
The doctor explained that a typical child would acknowledge he was in the room, and what Elizabeth was doing was a form of self-stimulatory behavior. More behaviors would follow, he said. Elizabeth might walk on her toes or flap her hands.
“She is so beautiful,” the doctor told Julie. “She will bring you so many years of joy.”
Elizabeth is fussy, and Julie can’t figure out why. The swings and pool usually keep her happy in the summer, but she wants something else and can’t tell her mom what it is.
She rubs her hands on her Strawberry Shortcake outfit, meaning she doesn’t want to wear it. The weight and texture of clothing are uncomfortable for Elizabeth, so she likes to walk around naked; sometimes she takes off her diaper. Her dad calls her Miss August.
Julie sewed this outfit herself—as well as four others—with lightweight cotton material. She put the zippers in back so Elizabeth couldn’t take them off.
Elizabeth leads her mom upstairs. Julie pulls a box of Pop-Tarts from the cabinet, but Elizabeth pushes it away. She stands in front of the refrigerator and starts to cry.
“What do you want, baby?” Julie asks. “What can I get for you? A graham cracker?”
She doesn’t want that. Julie picks her up to comfort her, and Elizabeth presses her face against her mom’s, wrapping her mouth around Julie’s chin. Some people who have autism crave deep pressure, the feeling they get from touching or holding. The pressure calms Elizabeth.
“I used to get really upset and frustrated when she’d get this way,” Julie says. “Then I realized it wasn’t helping her any to have two of us crying.”
Elizabeth gives up on the food and walks upstairs to William’s room. She lies on his bed and wraps herself in a sheet, then puts a toy in her mouth and stares at the ceiling fan.
Joe thought the neurologist at Children’s Hospital was wrong about Elizabeth. Some kids are late bloomers or just slow. He didn’t talk to Julie about the diagnosis.
“After a while, there is no denying it, and you have to take a second look at what you’ve been thinking,” Joe says. “It doesn’t happen overnight.”
Julie cried to a woman from her church for two hours. “At least she’s happy,” the woman said of Elizabeth.
What does that mean? Julie thought. At least she’s happy? She may never be able to talk.
Julie had always thought her kids would go to college. She’d pictured Elizabeth in the Little Miss Greenbelt Pageant singing “Somewhere Over the Rainbow.”
Now nobody could tell her what her daughter would be like in five years. There was no prognosis.
How could she have tried so hard to get pregnant and then have this happen?
“I’d be really mad at Joe because he wasn’t as sad as I was,” she says.
Joe lost his mother in his twenties; his father died of a heart attack soon after. Joe had a heart attack at 45, 15 years ago, and overheard a doctor say he had five to ten years to live. He’d learned to cope—turning to religion helped.
Soon after the diagnosis, Julie’s minister asked if she could come over. One day as Elizabeth slept, the minister laid her hands on the girl and prayed.
Julie thought William would be her little Einstein. He could recite the alphabet and count to 25 before he was two.
The plan was for William to start kindergarten at St. Hugh’s, a Catholic school connected to the parish Joe belongs to. William would go to DeMatha High School in Hyattsville, as one of his older half brothers had, then he’d study music or technology.
As Elizabeth was losing her language, William was learning hundreds of new words, like hippopotamus and umbrella. He knew train types: steam engine, diesel engine, gondola, boxcar.
But Julie started noticing oddities in his speech. Sometimes he sounded like a parrot: She’d ask, “Do you want a drink?” He’d respond, “Do you want a drink?” He’d use the same inflections as television characters—even a British accent. His speech seemed scripted, and he couldn’t hold a conversation.
Julie knew there was a chance William had autism. Studies show that a sibling of someone with autism—including a fraternal twin like William—has an 8-to-10-percent chance of having it. Identical twins have concordance rates as high as 90 percent, one reason researchers are confident that genetics play a role in autism.
Julie started writing down all of William’s words: How could he have a developmental disorder when he knew so much? She thought children with autism couldn’t speak—like Elizabeth.
She worked on flashcards with William as he lay in bed. She taught him the planets’ names and had him count coins until he fell asleep.
Sometimes Julie watched William as he slept. She had read that autistic children were diagnosed before they were three, so every morning she was eager to mark another day off the calendar.
We’ll make it through, she told herself. She felt as if she were sitting with a time bomb.
Most children show signs of autism by the time they’re 18 months old: A child might not gaze into a parent’s eyes, or might not smile back at someone.
“Typically developing babies are very engaged and interested in what you do,” says Dr. Rebecca Landa, who is researching autism in infancy. “Even at six to nine months, babies make an effort to get people’s attention.”
The National Institute of Child Health and Human Development publishes a list of possible “red flags” for autism. Among them: The child has poor eye contact, doesn’t respond to his or her name, doesn’t point or wave “bye-bye,” gets “stuck” doing the same things over and over.
A child doesn’t have to meet all the criteria. Someone can exhibit physical mannerisms and not have autism. Someone can have autism and make good eye contact.
Some parents hesitate to take their children to be screened because they aren’t seeing the “autistic” behaviors they expect. Others don’t want to believe their instincts.
“I wish people would get beyond thinking their child has to be 100-percent perfect,” says Julie. “I think they’re afraid, like I was afraid, to bring it up. If Elizabeth had cut her leg, I would have called a doctor immediately, but instead I see her crying and acting a little off and maybe staring into space—and those things I don’t do anything about.”
Although symptoms of autism typically appear before a child is three, many are diagnosed later. Researchers agree that children benefit from early detection. “We can actually teach two-year-olds with autism,” says Dr. Landa, who authored a study on development of infants with autism, recently published in the Journal of Child Psychology and Psychiatry . If children are diagnosed at 18 or 24 months instead of three or four years old, Landa says, they’re likely to have better outcomes.
Detecting autism in a child like William can be especially hard.
“Some may talk on time and show abilities like learning the alphabet, numbers, and how to match things, and understand cause/effect relationships,” Landa says. “They learn these things at an earlier age than expected, so parents think they’re really gifted.”
As the twins’ third birthday approached, William was still repeating himself and imitating his parents. Sometimes when he was excited, he’d scratch his fingertips on the floor. He didn’t know what to say when other kids talked to him.
Julie knew something was wrong, but she didn’t think it fit the classic description of autism. Neither did Joe.
She asked Joe to take William to a doctor—her husband hadn’t been in the room when Elizabeth was diagnosed.
“I wanted him to feel the same thing I’d felt,” says Julie. “I wanted him to grasp what was going on, because I felt like he was in such denial.”
Joe made an appointment with Dr. Conlon from Children’s Hospital. Julie asked Joe not to tell the doctor about Elizabeth—she didn’t want him making any assumptions.
Conlon said he suspected that William was on the high end of the autism spectrum. With an autism diagnosis, Julie realized, he’d get better services at school. He could be in an autism kindergarten instead of a regular special-education class.
“Part of me never wanted the diagnosis because I thought he just seemed a little quirky,” Julie says. “But if he didn’t get the diagnosis, he’d fall behind.”
Julie knew a mother and father who were fighting their son’s diagnosis and sending him to an expensive private school where he wouldn’t be called autistic. The father had said, “That label will follow him around for the rest of his life.”
After her autism diagnosis, Elizabeth was tested for Fragile X, a genetic disorder resulting from a gene mutation that can cause autism. She had an MRI of her brain, an EEG to rule out epilepsy, and a hearing evaluation. Every test came back negative.
When she was two, Elizabeth spent a year in the infant-and-toddler program at Beltsville’s Frances Fuchs Early Childhood Center before starting an all-day autism program with five other children. Her speech wasn’t improving. She had bladder infections, then kidney problems that went undetected for months because she couldn’t tell her parents what was hurting. She had started running from people—children who do this are often called “elopers”—a habit that scared Julie. Joe cried when he had to put a canopy over Elizabeth’s crib to keep her from getting out.
At school, Elizabeth learned to sort items into piles. She sat in her chair when she was supposed to. She starting using the Picture Exchange Communication System: A teacher showed her cards with pictures of food on them, such as Cheerios, and she was able to pick the one she wanted and hand that card to the teacher. Then the teacher gave her the food she’d asked for. Teachers at school called her “the smiling child.”
Elizabeth’s teacher recommended Floortime, a developmental therapy focused on child-directed interactions, introduced by Bethesda psychiatrist Stanley Greenspan, author of The Child With Special Needs . Greenspan believes that the therapy helps children learn to relate, communicate, and think. A parent or therapist spends 20 to 30 minutes interacting with a child on the floor in a play setting, following the child’s lead.
If Elizabeth wanted to communicate something, she’d have to get Julie’s attention. Floortime would create a back-and-forth.
Julie wants to find a buddy for William, someone he can talk to and learn from. When she sees a friendly child in the grocery store, she’s tempted to ask his parent, “Can he come over?”
William tries to play with Elizabeth, but she ignores him. If he puts his arms around her, she usually walks away.
In July, Julie took them on their first Metro ride, which William enjoyed, but Elizabeth plugged her ears and cried. A fear of sirens used to keep William from going outside; Elizabeth has trouble with loud mechanical noises. Sometimes it’s not the noise that bothers them; it’s the pitch.
Like many children with autism, they don’t like how certain foods look and feel. William likes potato chips, bread, cereal, and cheese and crackers, but the cheese has to be yellow. He stopped eating meat and peanut butter last year, so Julie puts a protein supplement in his milk. He won’t eat bananas, yogurt, or ice cream.
“It’s a texture thing,” Julie says. “He’ll put it in his mouth and start to chew it, and he can’t deal with it. If he watches someone else eating those things, he’ll get sick.”
His favorite meal is McDonald’s fries. Elizabeth won’t keep food on a plate and doesn’t use utensils. She’ll take a handful of William’s fries, eat a few, and throw the rest on the floor.
William occasionally takes his sister’s wrists and pulls her around. “Come on, Liz, come on,” he’ll say. “Ring around the rosie.”
“Joe and I have thought, ‘Should we stop him or shouldn’t we?’ ” Julie says. “We usually let it go until she tries to make him stop. I think it’s important that at least he try, and at least she try.”
When Elizabeth fell in the living room, William started crying: “What happened? What happened?” At school the next day, he said, “Her head. She hit her head. She hit her head. She hurts. She’s crying.”
If Elizabeth sounds as if she’s speaking, William praises her the same way her parents do. “Good talking!” he’ll say.
People tell Julie she’s lucky her kids don’t fight. Sometimes she’d rather they did.
After William was diagnosed in January 2005, he went through a screening and evaluation process called Child Find, which helps identify and refer children who need early intervention or special education.
The Child Find evaluators weren’t convinced William had autism. They placed him in a half-day special-education class at Francis Fuchs, Elizabeth’s school, with students who didn’t have autism. They wanted to see how he’d do.
William clung to Julie for the first week. He dropped to the ground and yelled, “Mommy, Mommy, don’t leave me!”
When Julie took him to Columbia Mall that summer, he couldn’t stop crying because of the noises and lights. A girl who worked there asked, “Does he have autism?”
Julie liked to think it wasn’t that obvious.
“Yes, he does,” she said.
“I could tell,” the girl said. “He doesn’t like those loud noises. Well, he’s still really cute.”
Julie couldn’t understand why people seemed surprised that a child with autism was cute.
At the end of the school year, William was still anxious when his mom dropped him off. He was doing more of his mannerisms—turning his hands inward and rubbing them against his stomach. Julie and Joe asked Dr. Conlon if medication or a change in diet might calm him. Conlon said yes but that medications came with side effects.
They decided they’d wait to see how William did in school that fall in an autism class with Timi Gray, his new teacher.
In the spring of 2005, Julie called Easter Seals to inquire about a program called Family Friends, which pairs older volunteers with families who have children with special needs.
That June, Julie met Ginny Jones, their “family friend.” Ginny, 59, had moved to Bowie and remarried. She didn’t know much about autism but wanted to work with kids.
As soon as they met, Elizabeth held Ginny’s hand and gave her hugs. William was scared—he kept saying “goodbye”—but Ginny assured him she wouldn’t touch him. The following week, William was showing her caterpillars. A week later, he told Julie, “She’s a fun lady.”
Ginny visits once a week. She pushes Elizabeth on the swings. William gets her to play “Sidney the Spider,” a tickling game. He takes pictures on her digital camera—she says he captures things she doesn’t see.
Ginny goes to the kids’ medical appointments with Julie and helps distract them. When Julie was nervous that William was bothering people in a waiting room—she often notices people staring—Ginny said, “Who cares what they think?”
Two summers ago, Julie took William and Elizabeth to Ginny’s house to go swimming. Ginny’s five-year-old granddaughter, Valerie, wanted to play with William.
“Grandma, he won’t talk to me,” she said. “I tried to get him to play, but he won’t.”
“William’s just very shy,” Ginny said. “When he’s ready, he’ll talk to you.”
Valerie walked over and said, “William, it’s okay—you can talk to me. Don’t be shy.” He didn’t say anything.
The next day, William was playing with two Little People toys, pretending they were talking to each other.
He made one say, “Don’t be shy. You can talk to me. Don’t be shy.”
The other responded, “I’m not shy.”
In 1999, Timi Gray was teaching children with disabilities in Prince George’s County when she was selected for a seven-week autism training. The county was creating autism programs and planning to start one at her school. They’d need a teacher.
Gray’s students had speech and language delays as well as learning disabilities. She had never met a child with autism. “They just came out of nowhere,” she says.
Once Gray started teaching kids with autism, she didn’t want to stop: “I would have six kids in the class all going their different ways, all in their own little world. That’s what made it challenging—I wanted to reach them.”
When Gray met William in the summer of 2005, he was shy and anxious. He followed along but rarely took part. He sat quietly. He’d say “fire truck” if he wanted one, but he was too nervous to get it himself.
“There was something about him that I had to get to the bottom of,” Gray says. “I knew he could do things, but I knew he was scared. So if I could just get him to feel comfortable, he’d be fine.”
Julie and Joe each came to the classroom to show William that school was a cool place. During one-on-one drills, Gray noticed that William wasn’t performing simple skills, such as putting beads together.
Julie videotaped William doing those tasks at home.
“He was talking to Julie and doing everything she said and answering her questions,” Gray says.
She started using the same language Julie did, and William recognized it. Gray realized that the tasks on William’s Individualized Education Program, a learning plan given to special-education students, were too easy for him.
“I didn’t push him,” she says. “I just took my time, and slowly he came out.”
Julie often thinks she hears Elizabeth say something, but because the words aren’t clear and her voice is soft, it’s hard to be sure. Elizabeth’s teacher said she talks when she’s frustrated—when a classmate had a ball she wanted, Elizabeth said “ball.” She yelled, “Daddy! Daddy!” during a blood test.
She was sitting at the dining table a year ago when Joe heard her say the first seven letters of the alphabet.
“It was out of the clear blue,” he says. “That’s the way her speech comes. You wonder: What the hell triggered that?”
Doctors tell Julie that the sounds are a good sign. “If she’s able to say it, it’s in there,” Dr. Conlon says, “but why aren’t we able to get it out?”
Julie used to look for the magic bullet. She was inundated by Internet claims: This therapy works! Try this diet!
She researched everything from Applied Behavior Analysis, a widely used set of principles that involves repetition and rewards, to nutritional therapies such as a gluten-and-casein-free diet, which eliminates proteins found in wheat, rye, oats, barley, and dairy products.
She read about “crystal children,” said to be highly sensitive children with penetrating eyes and delayed speech patterns who communicate telepathically.
“I think it’s parents grasping for anything to feel better,” says Julie. “I worry that it’s just a slippery slope away from tarot cards and paying people to come to your home and light candles.”
She saw a story on the Today show in 2003 about a little girl with autism who had starting talking at age three. The girl, Ashley, had been treated at Bethesda’s Spectrum Center, where she participated in the Tomatis Method of Auditory Training. The therapy, introduced in the 1950s by French physician Alfred Tomatis, is designed to reawaken the ear’s ability to listen. Using headphones, Ashley listened to music by Mozart as well as recordings of her mother’s voice, meant to simulate what she had heard in the womb. After two days of therapy, Ashley told her parents, “I want a cookie.”
Julie called the Spectrum Center that morning. She thought: This is my answer.
She signed Elizabeth up for Tomatis, but the $7,000 fee was steep, and insurance wouldn’t cover it. In the end, she and Joe decided against it. The same therapy wouldn’t work for everyone. And what if they found a way to pay for it and nothing changed?
They’re still not sure they made the right decision.
Timi Gray kept a poster on the chalkboard with a picture of every activity William and his four classmates would do that day and a time slot for each: circle time at 10:15, story time at 10:30, bathroom and walk at 11.
“The routine gives them security and stability,” Gray says. “When they come in here, they know what to expect.”
The structure helped William relax at school, but he still threw tantrums with his parents. His life wasn’t as regimented at home as it was at school.
Early in the school year, Gray suggested that Julie try a “first and then” board: Julie drove to places she typically takes the kids—the grocery store, the gas station, McDonald’s, and Target, William’s favorite. She took photographs of each place. She wrote the words “first” and “then” in big letters. She clipped them to the appropriate card.
“First we’re going to go to the gas station, then we’re going to go to the Target,” she told William.
“The anxiety and tantrums went out the window,” Julie says. “That was a wonderful day.”
Soon William didn’t need the cards. Gray encouraged Julie and Joe not to put him on medication—she said a drug might take his personality away.
It wasn’t long until William was waking up in the morning excited for school. “Let’s go see Miss Gray,” he’d say.
He started walking to the playground with a boy in his class. Sometimes he’d pretend he didn’t know an answer, just to see Gray’s reaction.
He picked words up quickly. Gray saw William point to the bottom of the doorway and ask his mother, “What’s that? What’s that?”
The next day at school, he picked up a truck, carried it to the doorway, and rolled it.
“Look, Ms. Gray,” he said. “Garbage truck over the threshold.”
Sometimes Julie has to ask William to stop playing on the Hot Wheels Web site so his sister can use the computer.
Elizabeth likes Reader Rabbit touch-screen games. She puts her face to the monitor and uses Julie’s finger to drag shapes into the spaces where they belong. She gets excited and clenches her fists.
One day last summer, Elizabeth didn’t ask for her mom’s hand. She put her own finger up to the screen and moved the shapes. “So good, Lizzie,” Julie said, tears in her eyes. “So good!”
Julie and Joe are relieved that Elizabeth is making progress again. Last year her teacher didn’t use touch-screen computer programs. She was stern with the kids—behavior Elizabeth wasn’t used to. Julie noticed her daughter changing: She would come home from school with her fingers in her ears and pull away from people.
Julie spent much of the summer doing Floortime with Elizabeth while William went to school with Gray. Every few weeks Julie and Elizabeth went to see Jake Greenspan—Dr. Greenspan’s son—for Floortime therapy sessions and parent coaching. Elizabeth liked having her mom to herself. She started showing Julie what she wanted to play with.
They listened to music and danced. Julie turned song lyrics into rhythms as they jumped up and down on the bed, and Elizabeth bounced to the beat.
Elizabeth started to laugh again as she had before. One morning in September, Julie and Joe awoke at 5 am to a little voice coming from down the hall.
“Twinkle, little, little star,” Elizabeth sang. “Dooka, dooka, dooka doo.”
There is no cure for autism or standard medication to treat it. Medications that treat other disorders—including anxiety, depression, and hyperactivity—can sometimes help alleviate symptoms and behaviors associated with autism. These include Prozac, Zoloft, and Ritalin. Risperdal, an antipsychotic medication, recently became the first drug approved by the FDA for the treatment of behaviors associated with autism in children and teens, including agitation and aggression.
Dr. Stephen Mott, chief of Georgetown University Hospital’s pediatric neurology division, credits the synthetic steriod Prednisone—not commonly used in patients who have autism—with helping nonverbal children start to talk.
Over the past seven years, Mott has prescribed the drug—often used to treat asthma, allergic reactions, and autoimmune diseases—to about 100 patients. Seventy percent showed improvement within eight weeks: Nonverbal children spoke. Patients who couldn’t put words together started using complex sentences. Some made better eye contact. A few bounced back from regressions.
Prednisone can cause serious side effects, including suppression of the immune system. A simple infection could become life-threatening.
Mott mentions Prednisone to patients in his list of treatment options, but he doesn’t push it. “It hasn’t undergone scientific scrutiny,” says Mott, who has treated patients with autism since the early 1990s. “I make that clear to families.”
Do the changes last?
“That’s the big question,” he says. Most patients continued with a lower dose, then the drug was tapered off. Of the 70 percent who improved early on, half later regressed to some degree. The other half kept getting better.
Julie used to wake up in the middle of the night with her heart pounding. She takes over-the-counter medication to help her sleep.
She misses going to church. She stopped because she didn’t feel William and Elizabeth were welcome at the Sunday service, and the church didn’t offer babysitting for special-needs children. Two women changed seats to get away from William.
Still, Julie considers herself fortunate. Some parents of children with autism don’t get to cuddle with them because their children don’t like to interact. Some kids hit people or try to injure themselves. Julie’s kids give her hugs. She’s trying to teach William what it means to say, “I love Daddy.”
The same thing that made her mad at Joe after Elizabeth’s diagnosis is what helps her now—his strength.
“He had a wonderful thing his father once told him,” Julie says. “ ‘You have to take care of your family—that’s just the way it is. You just do it.’ ”
The divorce rate among couples who have a child with a disability is higher than the average; there are estimates as high 80 percent. The stress is sometimes too much. Some spouses disagree on medical treatments.
“It’s hard enough for two people to take care of one disabled child,” Joe says. “Imagine one person taking care of two.”
He and Julie don’t agree on everything. She wanted to buy a harness for Elizabeth—William once ran away, and Julie caught him just before he reached a busy street—but Joe refused.
“He says it makes her look like a child on a leash,” Julie says. “My point is safety.”
Money is tight. Elizabeth and William are on a long waiting list for the Maryland Autism Waiver, which would make them eligible for respite care, medical coverage, and other services. Julie and Joe are hoping the waiver will help cover diaper costs, bars for the windows, and augmentative communication—a method that would allow Elizabeth to arrange pictures on a board to form sentences. They also want a new bedroom door with a Plexiglas window for Elizabeth, so they can close the door at night and let her sleep in a regular bed.
Julie and Joe have had five date-type nights out in five years. Elizabeth needs to be watched carefully: She once took a bite out of a wine glass. She likes banging pictures that have black in the frames.
The Arc of Prince George’s County, an organization that helps people with developmental disabilities, will provide assistance such as reimbursing families for a babysitter, but Julie and Joe say it’s hard to find someone they can trust. Two of William and Elizabeth’s godparents—a couple with whom Julie and Joe hoped to leave the children if something happened to them—stopped calling soon after Elizabeth’s diagnosis.
“Let’s play movies,” William says. It’s a summer afternoon, and he’s eager to sit inside the makeshift theater his mom created—a small tent covered with a bedsheet.
Julie is getting William ready to go see the animated movie Cars with his dad in a real movie theater. The last time William went to a movie, he got scared, and they had to leave. This time Julie wants him to know what to expect.
She crawls around the living-room floor gathering toy cars. “I hope we have all our characters here,” she says. “Nope—we’re missing Porscha.”
“You comfortable?” she asks.
“Comfortable,” William says. “ComÂfortable.”
She sets the scene: “William is at the movies. He’s with his daddy. He’s got his popcorn and his soda, and it’s going to get dark.”
She puts her hands under the sheet, as if at a puppet show. She gives each car a different voice and makes up dialogue.
William claps at the end and says, “Let’s watch it again! Let’s watch it again!”
A few weeks later, when Joe opens the door to the theater, William won’t go in. He wants to stay in the hallway. He doesn’t want popcorn.
Joe props the door open and sits in a spot where he and William can see each other. William comes in for previews, then leaves when Cars starts. It’s too loud.
Joe waves to him and checks on him, but he doesn’t want to move.
“Is he okay?” an employee asks
“He’s just a little shy,” Joe says.
William watches from the hallway for an hour before he says, “Let’s go home. I wanna go home.”
Joe’s happy. That’s longer than he’d expected.
At the end of last school year, Julie and Joe gave Ms. Gray a ring with a blue sapphire, the color of William’s eyes.
They’re thrilled with how far William has come since he started working with her and her support staff. He rarely throws tantrums. He went to a birthday party for the first time. He lets someone cut his hair.
When the family vacationed in Wisconsin in August, he went on a carousel and rode with Joe in a go-cart—things that used to terrify him. He won a second-place ribbon in Greenbelt’s Labor Day festival for a photograph he’d taken of a gazebo’s patterned-wood floor.
William made it through three innings of an Orioles game with Joe in September but wanted to leave after a player cracked his bat. He thought the batter would be upset.
“He broke the bat, he broke the bat,” William repeated. The cheering overwhelmed him. Sometimes William confuses his emotions: He’ll cry when good things happen—like when Jeff Gordon, his favorite NASCAR driver, wins a race.
He used to refer to himself as William, but he’s starting to use pronouns. He came home from school in the summer and showed Julie a piece of paper he was supposed to read. It had the words i see my written on it four times, with different pictures to end each sentence. Then he sounded out the words: “I see my backpack.”
When William broke a plastic racecar in September, he told his mom that Elizabeth had done it. He was nervously shifting his weight around.
Julie knew the truthÂ. She told William it wasn’t right to blame someone else for something he had done. She didn’t let him see how excited she was: He’d fibbed for the first time.
Julie drove William to see his new school, Beltsville Elementary, so he wouldn’t be surprised on the first day.
He talked himself through the change, the same way he’d seen Elmo do it on a back-to-school episode of Sesame Street: “Give Mommy a hug, say goodbye, and she’ll pick me up in the green van,” he said.
Gray told Julie that “self-talking” helps William figure things out. He verbalizes what other people do in their heads.
The first day, Julie put William’s backpack on him and he said goodbye. I can’t believe that just happened, she thought.
Julie came home to an empty house and didn’t know what to do. Elizabeth had taken the bus to her new school—Margaret Brent Regional in New Carrollton, a special-needs school where she can go until she’s 21.
William’s teacher sent home a note that day saying she thought he belonged in a regular kindergarten. He could do the same things other five-year-olds were doing except use the bathroom. William likes to sit, wipe, and flush, but he won’t actually go. His parents and his teachers are working on that.
Julie had hoped to have William in a mainstream class in a year or two, but she didn’t think it would happen so fast. He’d never been around typical kids. “It’s exciting but scary because he’s gone from this little quiet kid throwing up to just being so normal overnight,” says Julie. “It’s a shock. I want to just grab him and say, ‘Are you really sure you’re okay?’ ”
The teacher said the transition would be slow. He would have a classroom aide.
That night Julie told Joe, “We may actually have to think about saving for college.”
Julie has read that many adults with autism don’t marry. Why wouldn’t William get married? she thinks. He’s good-looking, smart, and funny: One morning he got out of bed and told her, “I’m not the Jedi I should be.”
She wonders whether William will live on his own or get a good job. She worries that people will take advantage of Elizabeth because she’s pretty and vulnerable. She and Joe are hopeful that if something happens to them, William can help care for his sister.
There’s no typical path for a teenager with autism. A low-functioning teen, with mild retardation, may continue to exhibit behaviors of a young child. A teen who is high-functioning might do well academically but struggle socially.
“I remember one child who had straight A’s and was an excellent brass player, but he did not have one friend,” Dr. Mott says. “He was fine with that. Some want to know why they don’t have friends and what a friend is, but there are others that are content with solitary behaviors.”
Some teens are teased and bullied. They don’t understand jokes or sarcasm and have trouble processing more than one thing at a time. Others blend in.
“Middle school is particularly hard because kids are getting to be so social,” says Roy Richard Grinker, author of Unstrange Minds: Remapping the World of Autism, out in January. “Kids with the social deficits of autism have a hard time functioning.”
Grinker, a George Washington University professor, has a 15-year-old daughter with autism who attends school in Montgomery County. “High school is much better,” he says. “The kids are more mature. They understand what autism is. The rise of autism awareness isn’t just some sign of crisis—it’s a sign that we’re finally understanding what all these people are like.”
Julie has heard that you can “test out” of autism—which she hopes might happen to William—though she realizes he’ll never actually be cured.
“In our clinic, in a small minority of cases, we will say to people, ‘Your child really no longer meets the criteria for this disorder,’ ” says Dr. Lauren Kenworthy, director of the Center for Autism Spectrum Disorders at Children’s Hospital. “We’re not saying they are perfectly normal right now, but we’re saying they’ve made so much progress.”
Julie recorded the 2006 ESPY Awards, for the best performances in sports, because the award for best moment of the year went to a teenager with autism.
Jason McElwain, a high-school senior who managed the basketball team, made six three-pointers in the last four minutes of a game. His team had a big lead, and the coach asked if he wanted to play. Teammates carried him off the court.
Julie didn’t like the way the media referred to McElwain as an “autistic basketball player.”
“Would you call a child with cancer ‘the cancer child’?” she says.
She watches the show over and over: “Every time I see him, I think he looks like Will, and he has the same enthusiasm.”
She and Joe have met only one adult with autism—a man named Dennis who came to their house to look at a train collection Joe had listed in the paper.
Julie introduced herself, and Dennis averted his eyes. He looked like a college professor. He worked at NASA.
Sometimes Dennis spoke Latin. He talked to Joe about Poland, where Joe’s ancestors are from, and about God.
“He spoke like you could jump into his world and know what he knew,” Julie says. “That’s what William does.”
Julie had an uneasy feeling around him, which made her mad at herself.
Dennis was fascinated when Julie said her kids had autism.
“William, did you ever do this?” he asked, patting his head. “When I was your age, my thing was patting men’s heads. I was told it wasn’t socially acceptable.”
Julie had mixed emotions about the visit. Here was an intelligent man making it in the world. But he was a landscaper.
“When he said he worked at NASA,” Julie says, “I thought he was an engineer.”
The water in Ginny’s pool is cold, but William and Elizabeth don’t mind. William helps blow up his Cars floaties for his arms, gets in, and does his scary shark voice.
“Washing machine!” he says. Ginny lifts him up and down as she sings, “Washing machine, washing machine, we have to make the clothes all clean.”
Elizabeth splashes in the water like any little girl who’s big enough to stand but doesn’t know how to swim. She jumps off a low ledge just as William does. She opens her mouth and keeps swallowing water.
“De-licious!” William says.
When Elizabeth takes her floaties off, William brings them to her. “She needs to have them on,” he says. “Put them on, Lizzie.” Ginny tells Julie to let Elizabeth swim without them: She’ll be fine.
Julie looks around and sees Elizabeth playing without her floaties and William wearing goggles that make his nose look funny.
She can’t stop laughing. It’s the first time she’s felt this relaxed in a while. Her kids are having fun in a swimming pool, doing what kids do.