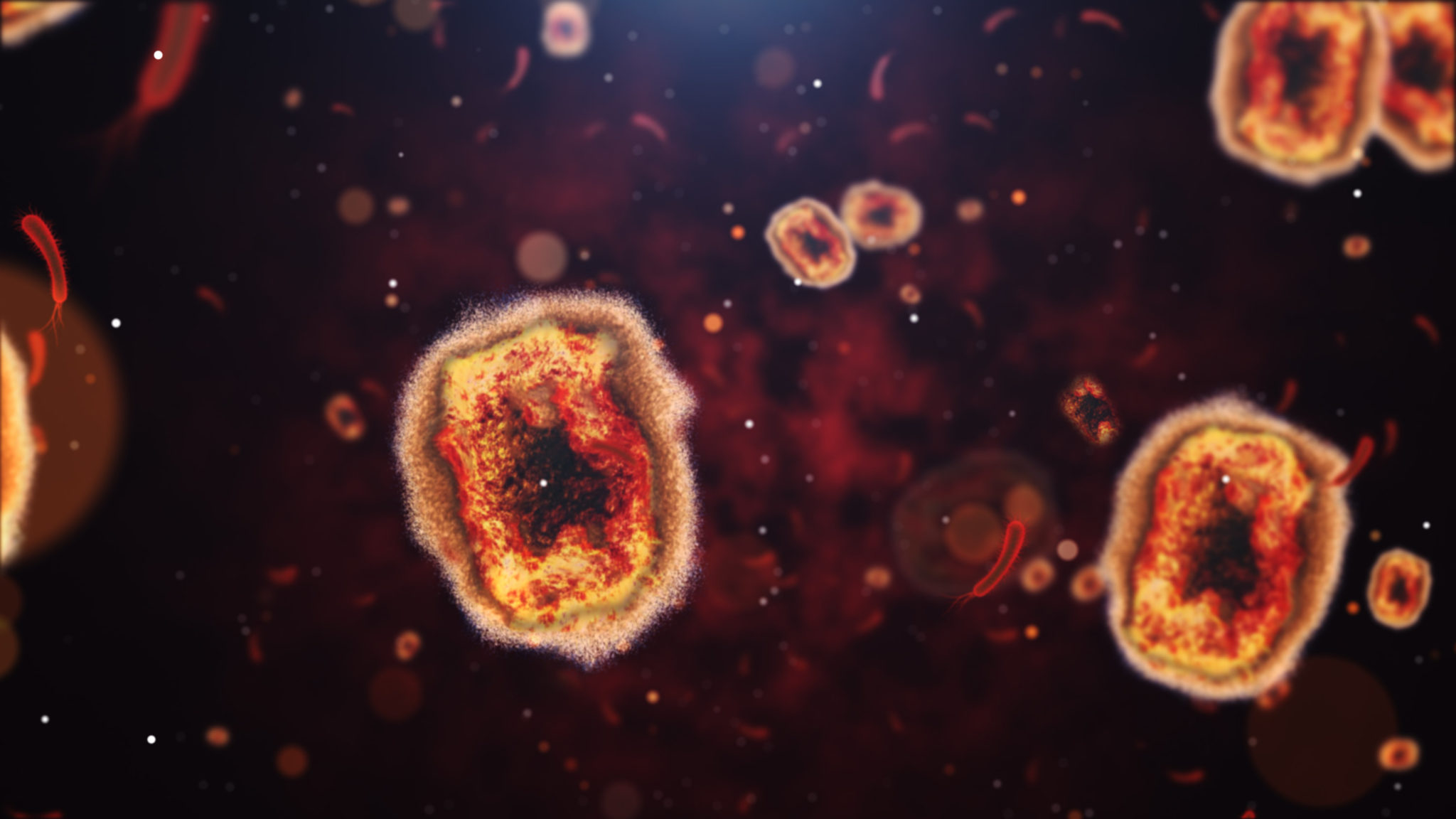
DC has more than 300 cases of monkeypox. Last week, the US declared the virus a health emergency and the city’s health department began to offer limited walk-up appointments for monkeypox vaccinations.
We spoke with Carlos Rodriguez-Diaz, an associate professor of prevention and community health at George Washington University’s Milken Institute School of Public Health, about what monkeypox is, what it looks like, and what Washingtonians should be aware of as cases rise.
Washingtonian: What is monkeypox?
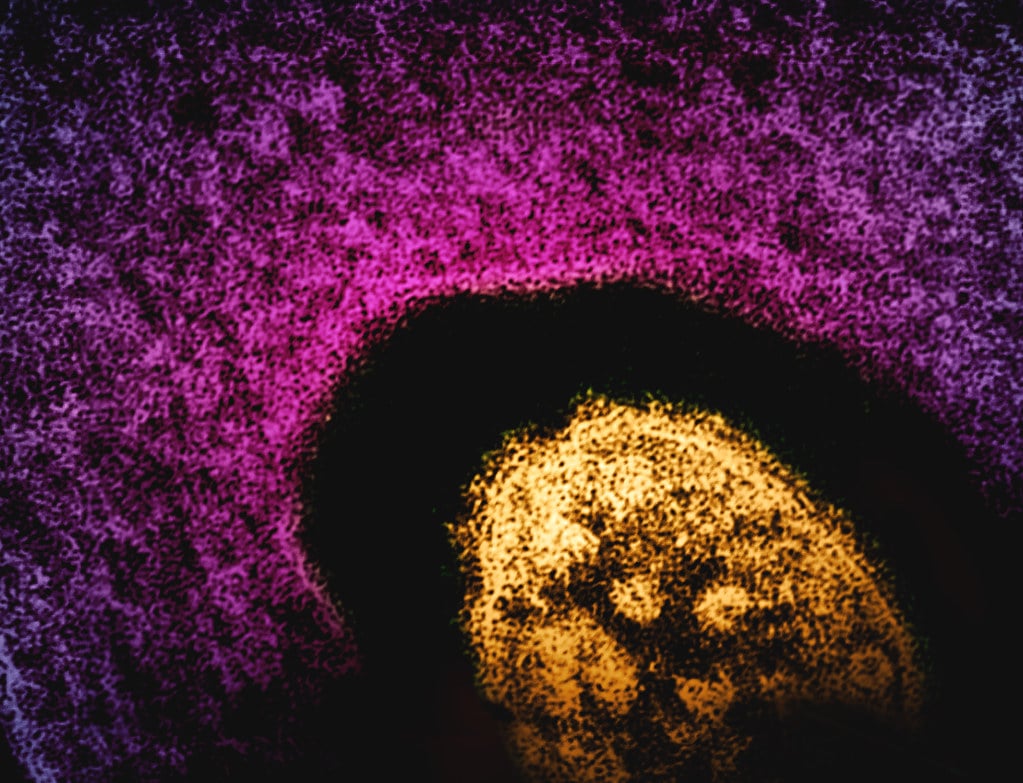
Carlos Rodriguez-Diaz: Monkeypox is part of a community of viruses, including the virus that causes smallpox. The symptoms are similar, but milder, and monkeypox is rarely fatal.
We have known about monkeypox for decades and currently it is endemic in some countries in central Africa. What we’ve seen more recently is a mutation of the virus that has been transmitted human to human. The initial cases were in the United Kingdom and have spread to Europe and the Americas. We have cases in more than 80 countries in the world right now.
Why has the virus started to spread to so many countries?
Decades ago, we stopped using vaccines to prevent the virus because it was basically eradicated from most countries. That has created a susceptibility now.
What are the symptoms?
Some people are not showing many symptoms until they see some of the rash, or scabs, on different parts of the body. Other symptoms include fever, chills, swollen lymph nodes, exhaustion, and general muscle, back, and headaches.
How does it spread?
The easiest way is skin-to-skin contact with a person who has the infection and has symptoms. The current outbreak—more than 90 percent of cases—is happening in networks of men who have sex with men. It’s been described as a sexually transmitted infection, but we don’t have enough research to say that it is in sexual fluids. It’s being transmitted because when we have sex, we touch each other, and that’s the easiest way for the virus to be transmitted.
It is also possible to transmit the virus through clothes or [bedding] that have been used by a person who has the infection and has symptoms. Additionally, transmission depends on where the person has lesions or blisters. Transmission may take less time if the person touches one of the infected lesions. The virus is not airborne, but can sometimes spread through respiratory secretions, like mucus, so mask-wearing could help lower the risk of infection.
Why is it impacting men who have sex with men specifically?
Our hypothesis is that the infection started affecting sexual networks. People have sex, and they have sex with other people, and as people keep getting in contact sexually or continue sharing clothing or bedding, then it remains in those circles.
Why is Washington a hotspot for cases right now?
DC is one of the cities with a high concentration of members of the LGBTQ community, so that’s the correlation. That’s why it’s also happening in other so-called gay enclaves like San Fransisco, New York City, or Chicago.
How concerned should people be?
The strategy is to contain the outbreak. We need to provide resources to the groups the virus is affecting the most so they can get tested, they can get the vaccine, and if they get infected, they can get the treatment that they need. Men who have sex with men are not limited to interact with other men who have sex with men—they go to work, they go to social events, they have families. If we respond on time and are able to contain the infection and provide resources to these communities, we’re going to be fine. Otherwise, we’re going to see it spread to other sectors of the community.
It’s very likely that soon we’ll see cases outside of people who identify as men who have sex with men or within the LGBTQ community, but we can contain that. Right now, people who are not gay or bisexual should not be concerned that they don’t have access to vaccines because that is not the public health recommendation. If we get to that point, we will have new recommendations and we will be able to provide more information about resources and what to do.
How can people protect themselves?
We need to focus on people who are at increased risk. For gay, bisexual, and other men who have sex with men, we are recommending harm reduction. If they can reduce the amount of sexual partners or can engage in conversation with their sexual partners in terms of the risk associated with the infection, that will be extremely helpful to reduce new cases.
We are also encouraging men who have sex with men to get the vaccine. The vaccine, at least here in DC, is available and it’s free. If someone has symptoms, we recommend they contact their primary healthcare provider right away and get tested. If they’re contacted by health authorities that they’ve been in contact with someone who tested positive, they may be asked to stay at home for several days so we encourage them to comply with those requests.
What misconceptions have you seen about monkeypox?
We need to avoid stigmatizing certain groups. It just happened that this started among gay men. But it’s an infection that could affect any human.
Within the public health response, I think we can also do better to address the issues that are affecting gay men and men who have sex with men. We knew before the pandemic that there were disparities because of race. Covid-19 only made them clearer. We need to make sure that the resources are available for everybody who needs them right now. That includes flexible schedules for the vaccine, more walk-in clinics, and more information available in Spanish and for people with low levels of health literacy.