Related:
How to Cure Insomnia at Home
Sleep Centers in Washington
Finding the Perfect Mattress
Sleeping overnight in an office building is not my idea of a good time. But it seemed to be the only way to figure out why I was always sleepy—head-nodding, please-may-I-put-my-head-on-the-desk sleepy—when I needed to be alert, such as at work or while driving.
So I was walking into a Chevy Chase high-rise at 8:30 pm, pajamas in hand. Maybe the experts at the Center for Sleep & Wake Disorders could tell me why I wanted to crawl back into bed soon after waking. On the 17th floor, the sleep techs awaited my arrival.
Nearly seven in ten people in the United States say they don’t get enough sleep, according to the National Sleep Foundation. The most common disturbance that sleep labs diagnose is apnea, which—along with restless-leg syndrome, narcolepsy, and other disorders—can be treated with medications or special gear. Even if problems can’t be cured, most can be managed.
A technician at the reception desk hands me paperwork to fill out, and another shows me to my room. The clinician who recommended the sleep test told me the sleep center was just like a hotel. And it is, once you remove the carpeting, the television, the room-service menu, the full-size bed, the mini-bar, the little soaps and shampoos, the drapes, and the window. And then put the bathroom in the hallway.
I’m nervous about how the evening will unfold—a feeling that doesn’t bode well for falling into a nice, deep sleep.
A technician arrives with a bunch of equipment, most of which is going to end up on me. She takes a jar of paste and affixes pads with wires to my forehead, scalp, chest, back, legs, and arms. “Let us know when you’re ready to go to sleep and we’ll plug you in,” she says.
I climb into the twin bed with its single pillow and start to read. At about 11 pm, I pad across the hall to the bathroom so I don’t have to make the trip—wires and all—in the middle of the night. Then it’s time. A sleep technician plugs me into a box on the nightstand. He shuts the door, and I turn off my bedside light. It’s hard not to think about the fact that the technicians can see my every move on their monitors. And hear everything, too.
I don’t fall asleep quickly, and I don’t sleep well. I wake up several times, but I’m afraid to move much for fear of pulling out wires. I end up having to call someone to unplug me for a bathroom visit. It’s not a soothing evening. In the morning, a technician detaches me from the gear. I shower, then head for work.
When people first hear about sleep labs, many believe they’ll be packed with insomniacs. Not so. Sleep labs are set up to look for problems that wake you up or cause you to sleep badly, leaving you tired. Doctors won’t keep you overnight to see why you’re not falling asleep. The focus is on evaluating your ability to maintain sleep once you’re down and out.
Even non-insomniacs can have problems dropping off to sleep on the night of a sleep test, as I discovered. What no one told me beforehand is that the doctors aren’t out to see a perfect night’s sleep, so I shouldn’t have been anxious about my performance.
The techs need only witness a few hours of “representative” sleep to determine obvious issues. They expect that it will be hard for many people to sleep. Sometimes, doctors administer a sedative to help someone nod off. That may affect the test to some degree, but “it’s a choice between some data or no data,” says Dr. Lawrence Stein of Pulmonary and Medical Associates of Northern Virginia.
A sleep lab isn’t the first stop for troubled sleepers. First, a doctor assesses what a patient’s life is like while awake. Some people simply don’t allocate enough time to sleep, Stein says. “Insufficient-sleep syndrome” is a common phenomenon. Most people need about eight hours, and if they don’t fit those in because they’re busy doing other things, they may be chronically fatigued.
Sleep dysfunction often is related to other medical conditions. Doctors taking a clinical history look for anemia, depression, thyroid problems, and other matters and treat those before resorting to an overnighter. Dr. Helene Emsellem, the Chevy Chase center’s medical director, also asks patients about lung, skeletal, sinus, neurological, and psychological issues.
She also has patients fill out sleep logs and asks them to practice better sleep hygiene, such as cutting out caffeine after 2 pm and keeping their weekend sleep schedule closer to their weekday hours. The brain can shift its expected sleep cycle by only about 1½ hours before sleep gets disrupted. She also suggests people set aside time to wind down after a busy day, even if it’s only 15 minutes: “Take a warm shower, do some gentle stretches, a little light reading.” Basically, set the stage for sleep.
It’s usually when there’s no obvious reason for daytime drowsiness that a doctor orders a sleep test. At the lab, personnel look for breathing disturbances, limb movements, acting out a dream. The wires monitor brainwave activity, eye movements, teeth grinding, chest movement, air flow, and more.
There are clues that something’s gone amiss during the sleep hours. You’re sleepy during the day. Your spouse or partner tells you that you snore. You gasp for breath in the middle of the night. The bedding that was hospital-corner snug in the evening is a disheveled mess in the morning. Your mouth is dry.
Whom should you see for sleep issues? It depends. The physicians who diagnose sleep problems come from a mix of disciplines. Emsellem is a neurologist, while Stein is a pulmonologist. Dentists, psychologists, and ear-nose-and-throat doctors may also be board-certified in sleep medicine.
Because my sleep test was mostly a blur, I decide to observe a test on someone else while I stay awake. Stein arranges for me to visit the sleep lab at Virginia Hospital Center. In a half-darkened waiting room on the second floor, a woman sits with an overnight bag and two large pillows. A guy leaning against the wall says, “I hope I can sleep.”
The registered polysomnography technicians get their patients and go to work prepping. One of them, Tauseef Dilawari, is wiring Trey Eckels, 36, from Alexandria. A strap around the torso. A heart-rate monitor on his finger. A plastic tube under his nose.
Dilawari leaves the room to test the equipment. From an intercom, she tells Eckels to move his eyes this way and that, grind his teeth, breathe deeply in through his nose and out through mouth. Flex each of his legs up and down as he would on a gas pedal. Then right and left.
She tells him that if he stops breathing 20 times within an hour or his oxygen is low during the night, she’ll wake him and put a CPAP—or Continuous Positive Airway Pressure—mask on him. It’s a device used to treat sleep apnea. The word “apnea” comes from the Greek for “without breath.” Obstructive sleep apnea, the most common type, is caused when the airway is blocked, usually when the soft tissue in the back of the throat collapses and closes while you’re sleeping.
I watch Eckels try on a bunch of masks. He says the mask isn’t going to be very romantic for his girlfriend.
“Bring her in,” Dilawari says. “We’ll put one on her, too.”
Dilawari has seen some unusual things in sleep labs. People have come in with humidifiers, quilts, stuffed animals, and noise machines. One woman brought a large suitcase packed with linens and stripped the bed when she arrived. Another was accompanied by her husband, who told her a bedtime story before lights out. A guy came in with a six-pack of beer. And one sleep-deprived sheriff showed up with four guns because he couldn’t leave them in the car overnight.
Once doctors diagnose a sleep disorder, they recommend treatments. The CPAP can work miracles for apnea patients, but it can be a challenge to get some to wear the mask. Says Stein: “Fifty percent love it and use it frequently. Twenty-five to 30 percent won’t use it no matter what you do.” The rest use it some of the time, and when they do, they function better the next day.
As for me? My legs aren’t restless, and I don’t have apnea. But during my test, I did cycle into REM sleep later than average and had 97 minutes of awake time. I took a daytime sleep test and was able to nap successfully every two hours, nodding off in an average of six minutes. I’m a good sleeper! But only during the day.
I fall into the category of “too sleepy for no discernible reason,” a.k.a. idiopathic hypersomnia. Some people simply are tired no matter how much sleep they get. “The brain does not generate adequate awake signals during the day,” Emsellem explains. She’s hopeful that someday the secrets will be unlocked.
She doesn’t leave me completely high and dry. One way to manage unexplained daytime sleepiness is with a “wake-promoting agent” such as the stimulant Ritalin. I’ve got a meeting at 11 am today. Pass me the meds, please.
This article first appeared in the January 2011 issue of The Washingtonian.
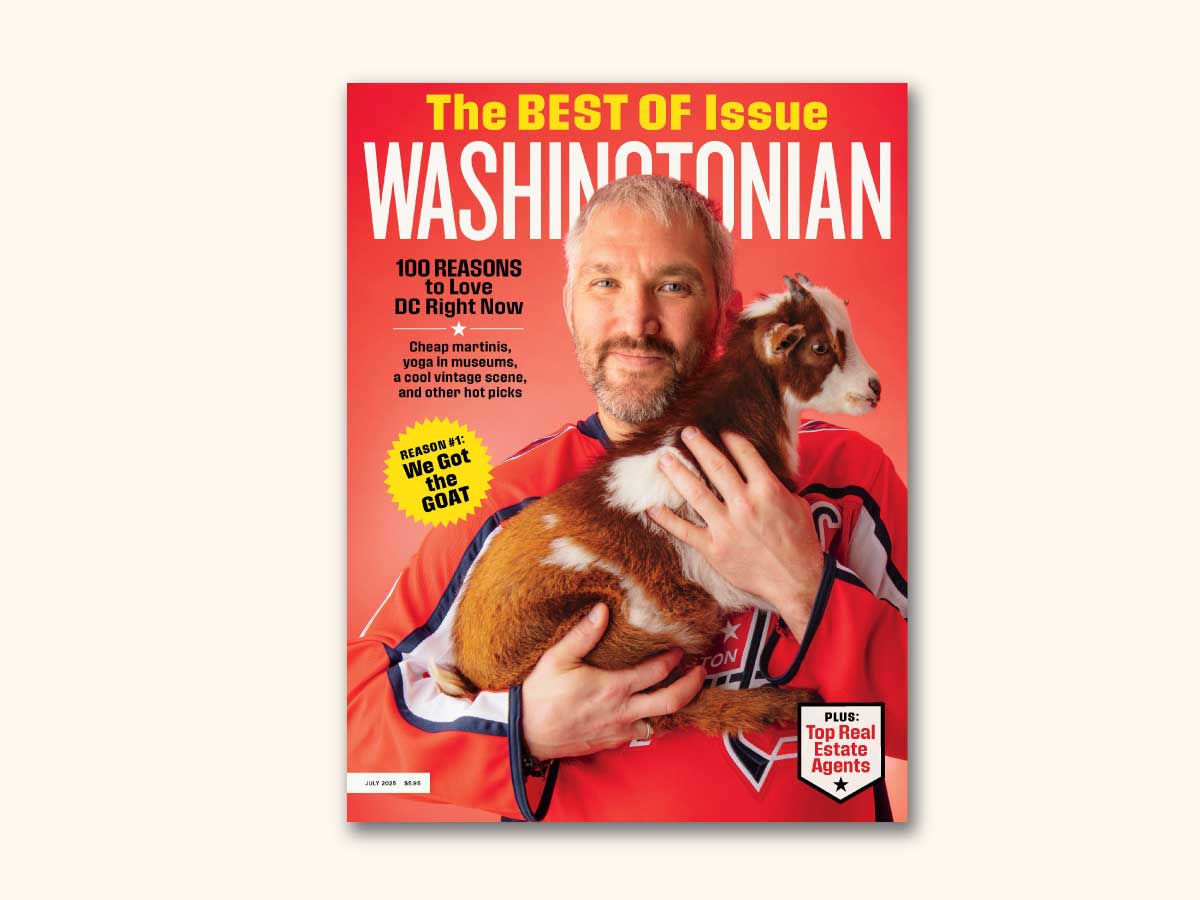
Subscribe to Washingtonian
Follow Washingtonian on Twitter
More >> Health | Top Doctors | Well+Being Blog