In the summer of 2019, a flurry of articles appeared in the press in rapid succession. They each described what healthcare experts were warning was a fast-approaching disaster: a “devastating” shortage of doctors in the United States.
Just months later, amid the coronavirus pandemic, shortages (and exhaustion) among doctors and nurses have never been more acute. As a response, plenty of ideas have gained traction: adding to the PPE stockpile to protect hospital workers, adding fourth-year medical students to hospital ranks—even adding more immigrant physicians.
But what about the idea of simply producing more doctors?
Many Americans may not know that the number of doctors is essentially set by Congress. Each year, the Centers for Medicare & Medicaid Services, or CMS, provides payments to hospitals to hire their residents—the crucial bridge that medical school students must take to becoming licensed physicians. Because the number of residencies is tantamount to the final number of doctors, the federal government has enormous leverage over the number of new physicians that enter medicine each year.
But the number of new residencies for which the federal government pays has not budged in twenty years. In 1997, Congress passed the Balanced Budget Act, a bipartisan effort to cut back on spending. The act put a cap on the number of annual residencies CMS would support, and froze the funding at 1996 levels.
Within years, medical experts began warning that a doctor shortage was in the offing. Since 2007, a bill to increase the number of residencies has been introduced in every Congress—including five times by Joe Crowley of New York, who was later defeated by Alexandria Ocasio-Cortez—but never passed. Last year, the Resident Physician Shortage Reduction Act of 2019 was proposed by Terri Sewell, a Democrat from Alabama, which would increase the number of residencies by about 3,000 for five years. It also grants the Secretary of Health and Human Services flexibility to determine to which regions those residents will go, since geography is a key aspect of the country’s shortage.
Sewell’s measure would make a big dent. But the aggregate increase in doctors would only amount to about 15,000. According to the Association of American Medical Colleges—the country’s leading advocates for lifting the residency cap—the shortage of total physicians by 2032 is projected to be between 46,900 and 121,900. At least half of that shortage is expected to be among primary care physicians alone.
In an interview edited for length and clarity, Dr. Janis Orlowski, the AAMC’s Chief Health Care Officer, explains the history of the doctor shortage, why the problem demands a legislative solution, and whether Congress should be involved in producing doctors at all.
So how did we get stuck with this problem? And how did we end up with Medicare basically determining the number of new doctors per year?
Dr. Orlowski: So, let’s start at the basics. Today, many people take a look at the number of physicians per 10,000 people—we have always been lower than other countries. And in this pandemic, it’s interesting to note that the number of physicians we have per 10,000 people is substantially lower than, say, Italy’s number of physicians for their population. So we’ve had a lower number, and that’s sort of a starter.
The second thing that’s happened, the AAMC and others have looked at the workforce and said, what do we need for the future? To become a doctor, you go to college, four years medical school, then you do a residency, and that can be anywhere from three to six years. Sometimes longer, if you go on to sub-specialize.
When Medicare came out maybe 53 years ago, the [Johnson] administration said: Holy cow—we’re going to have insurance for all of these older people, so we better make sure we have doctors.
And so the funding [of residencies] came in the 1960s with the Medicare Act. You know, I think it was very reasonable at that time: We’re going to give people Medicare, we’ve got to make sure we have doctors who can care for them. And in the forties and fifties, people didn’t see doctors in the same way we do now. What [Medicare] did was help push specialty care—and oncology care and cardiac care—forward to the levels that we have now. So there are many wonderful benefits from that decision to include funding [residencies] in the Medicare program.
Then Congress passes a law in 1997. And at the time, the AAMC endorsed the bill, right? Why was that?
So the 1997 act froze the number of residency slots in the country. It was part of the Balanced Budget Act.
At the time, everyone’s idea was that [residency funding] was going to be put on hold for a year or two, then reassessed. … If you look at the testimony, it’s very clear.
So dial a couple years after that. In 2003, the AAMC said, we are going to need more doctors, for two main reasons. One is, if you take a look at the US census, the population of the country continues to grow, at a point where it has outstripped the number of doctors that we’re likely to have in the future.
We continue to say to people: You can’t go out and grow a doctor in a month.
And the second big reason was the fact that we had the aging of the Baby Boomers. What we know is that when you’re 30, you might see one doctor, or a second. But once you’re older than 65, you tend to see multiple doctors in a year—you might see your primary care physician, a cardiologist, a surgeon, a gastrointestinal doctor. The number of doctors goes up.
So as we continued to look at the statistics, what we said was, there’s not enough doctors for the growth of the US population, and the aging of the population.
And what was the push for action at that time? Was it clear from the beginning that we needed a legislative response?
It was talked about, it was discussed—“We need more doctors”—and then you see two things. One is, the number of planned medical schools goes up. We’ve gone from about 120-some medical schools in the United States up to 155.
The second thing is, a number of [schools] looked at their class size and said we’ve got to expand our class size. And they have, from 2003 to now….And so, medical school applications are up and matriculations are up—35 percent, it looks like this year. So what we’re saying is, we’ve done our part.
But there’s the residency cap.
We’re just bumping up against it now. Before, there was a gap [between American medical students and the cap limit]. That gap was filled by international medical graduates. So if you take a look at the US right now, about one out of five physicians are foreign-born. We essentially have had to count foreign doctors coming to the United States in order to continue to grow our healthcare delivery system. And now our American number of graduates is bumping up against that cap.
So back to Congress, then. How long have they had to deal with this issue? And why has it dragged out so long?
The interesting thing is, in the Affordable Care Act, they said, Holy cow—if we’re going to give all of these uninsured people insurance, we better have enough doctors for them. And there was a clause in the ACA to increase funding for physicians, but it never passed.
I believe there’s been legislative bills that have been presented to the House over the last ten years at least. And there has been bipartisan support—until it’s gotten to the dollars, to the money. And we’ve never made it over that hump.
Meanwhile, hospitals have continued to slowly increase the number of residency slots they’re paying for themselves. And you know, that’s not going to continue. When you take a look at the pandemic we’re going through right now, if a CFO takes a look and says, should I pay for two more resident slots? Or do I have to get more PPE?
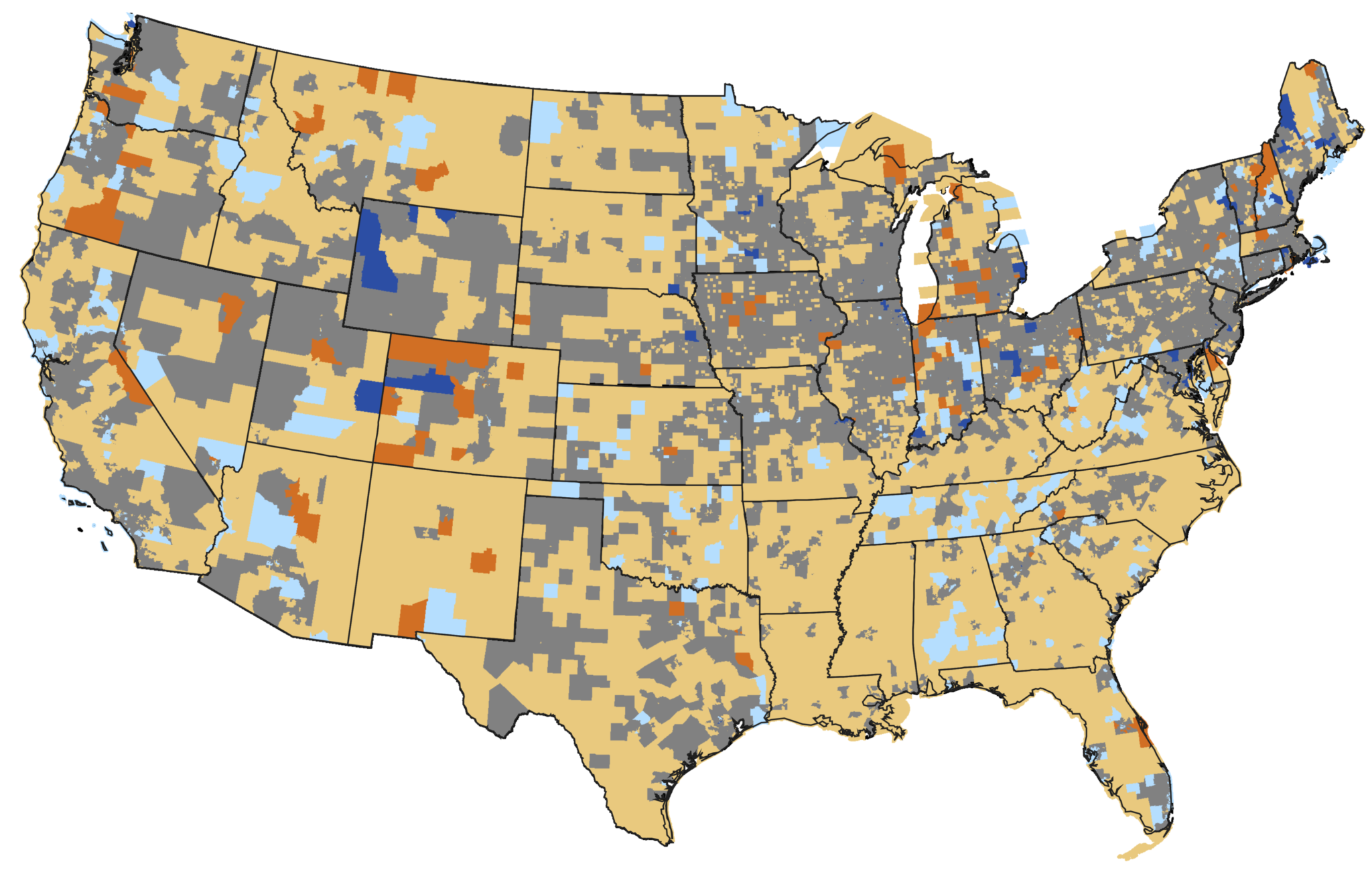
In the end, it’s part of the US not thinking ahead, and not being prepared. We continue to say to people: You can’t go out and grow a doctor in a month. We’ve got to have some forethought, we have to plan. Not only has the AAMC been saying this, but HRSA [the Health Resources & Services Administration], which does the workforce numbers for the government, has been saying there’s a shortage. You take a look at the map, sure enough, we’re short of doctors in all these different areas.
So why hasn’t it [moved] forward? I think it’s the will to keep yourself prepared, and to make the hard decision. If you take a look at the preparedness money that was given to hospitals and healths systems five years ago—when Ebola was considered to be the thing that we needed to worry about—it’s down to a trickle of dollars right now, because we’re at the end of the five years. Certain agencies that worked on these issues have been closed, or assimilated into other places. So we act when there’s a crisis, but we don’t act with preparedness. I think the physician shortage is one of those stories.
The obvious question is whether the pandemic will give a boost to this idea in Congress. Is it safe to say that?
We are trying to be careful on the pandemic. We don’t want to use the fact that doctors and nurses are on the front line, and some of them are dying on the front front line—we don’t want to look like, Oh, now’s the time to ask for money. We want to say: This has been a long time. We have a very studied view of workforce shortages. We’re not coming out today saying, “Guess what!” What we’re trying to do is highlight that this has been a discussion, that should have been part of the American people’s discussion on what they want to pay for and what they want in terms of preparedness.
Could the pandemic backfire on this idea? Say the public sees this crisis as a shortage of specialists—ICU doctors, intensivists, hospital workers. But your report says the shortage is everywhere, and at least half the problem is primary care doctors [i.e. non-specialists]. Could we come out of this crisis funding the wrong doctors?
What I would say is that there’s a role for everyone. We should not be myopic and say, we’re just going to grow Nurse Practitioners. As you see in this pandemic, we need the specialists, we need the pulmonary specialists, we need the critical care specialists. So we need to have the breadth of speciality. People say, ‘Is there still a PCP shortage, and are those the doctors that we need?’ I always say, there is a PCP shortage—but you know, in the opioid epidemic, what came out was that we have a shortage of behavioral health [specialists], we have a shortage of psychiatrists, people who work with pain and substance abuse. You can tell right now with some of the specialists, we have shortages. And so it’s not, ‘Do we have a primary care shortage?’ We have a primary care shortage, and we need these other doctors. And the crises that we’ve gone through point out some of these physicians that we need.
There are people who argue for phasing out the Medicare med-school payment system altogether. If it takes Congress 20 years to get around to lifting this cap, isn’t it fair to ask why a gridlocked legislature has anything to do with producing doctors?
You know, the question has come up—it shouldn’t be Medicare, it should be the federal government, it should be the states through Medicaid, insurance companies. Or we should have an all-payer fund. Daniel Patrick Moynihan from New York was one of the people who tried to argue, let’s just not make this a Medicare issue, let’s make this an all-payer program. That didn’t happen.
So there have been discussions about, is [Medicare] the right place for residency funding, and what else do we do? What ends up happening is that when there’s not enough money, and you have a stream of dollars, people fight to preserve funding. They don’t trust that if they [remove] Medicare dollars that we’ll look for another place to fund the residencies. And you know, you have to show [them] where that place is, before they’re going to feel comfortable. The reason is because in 1997, they said we’re going to pause this for two years and think about it. And there’s been no action.
One last thought. There’s a part of our report that talks about inequity, and utilization. I was just on a phone call that had to do with inequities in the incidents of Covid-19—particularly in minority populations, and their higher deaths. How do we bring healthcare to these areas? You take a look at our workforce report, and pay attention to the fact that this workforce report says [what will happen] if things continue as they are. But we are not advocating for things to stay as they are. We’re advocating for everyone to have better access to physicians.