It’s 10 o’clock on a Monday morning, and the phones are ringing at Bristol Women’s Health. “Do you know the first day of your last menstrual cycle?” asks Krystal Biggs, wearing a black headset over her reddish dyed braid. “Looks like you’re just about four weeks, so we’d be able to do the medication abortion. Was there any particular day that you’d want to come in next week?”
As Biggs takes down the patient’s information, Stephanie Rosenwinge is putting out fires: The water fountain in the hall sprang a leak overnight, and the heat did something wonky—it’s 50 degrees inside, and it needs to be comfortable before patients arrive. Rosenwinge, 55, wears clear-framed glasses, a graying ponytail, and a shirt that says “My Uterus Is Committing Crimes Right Now.” All morning, she’s been dashing around the cavernous building, a former hearing center in southwestern Virginia that was repurposed as an abortion clinic in July.
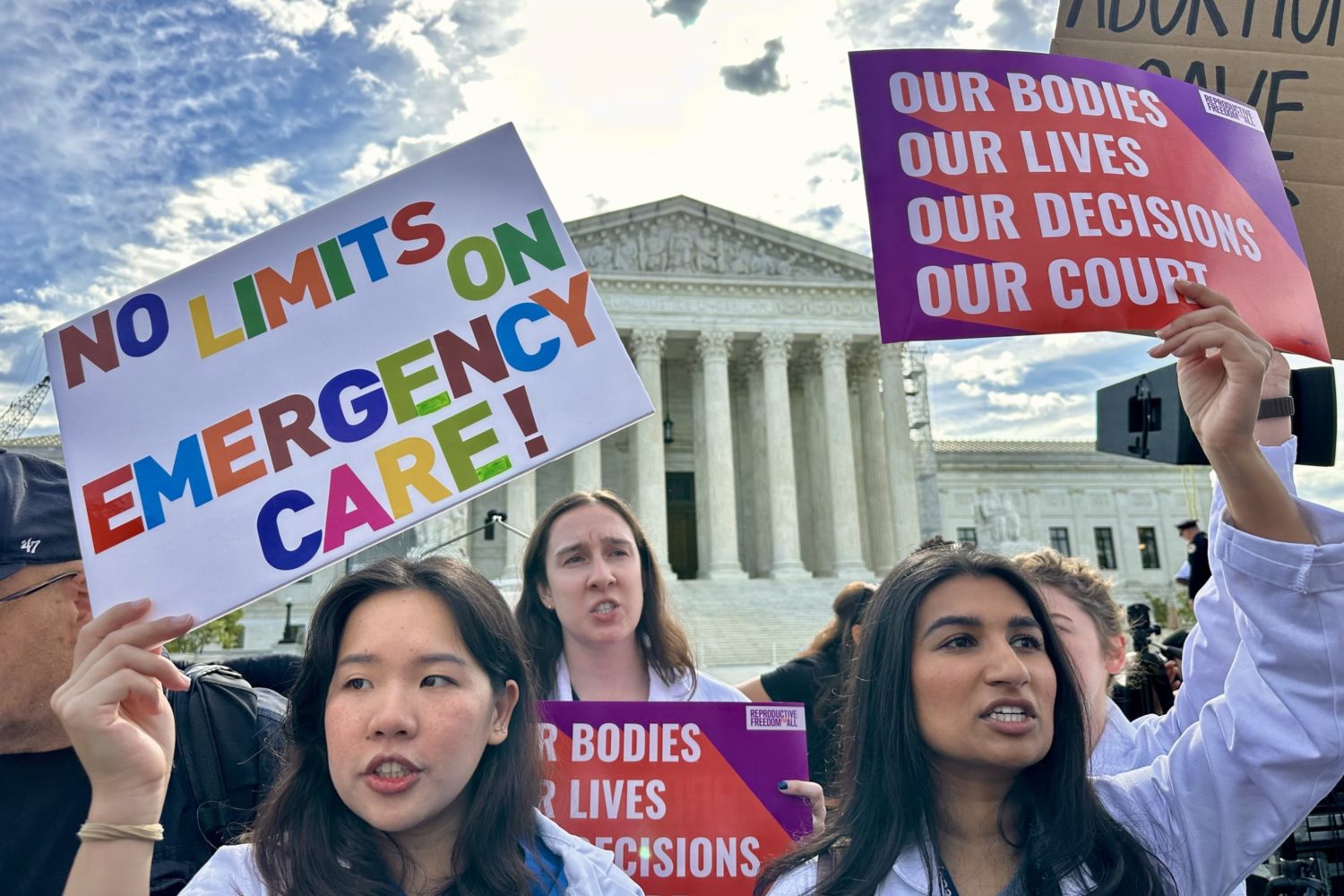
Bristol is a twin city, half in Tennessee and half in Virginia, bisected by the main commercial strip downtown. But in June, when the Supreme Court overturned Roe v. Wade, eliminating the constitutional right to abortion, it created an absurdity: Abortion remained legal on the Virginia side of town but not on the Tennessee side, where a doctor had been offering abortions for more than 40 years. Unbowed, he rushed to open a new clinic—Bristol Women’s Health—about a mile up the road in Virginia. This has been one effect of the fall of Roe: clinics springing up on state borders in places where abortion access is scarce, part of what Rosenwinge calls the “intense scramble to get care for the women of the South.”
On this November morning, Rosenwinge flies through her to-do list—sop the leak with paper towels, warm the gel for the ultrasound machines, stock the bathrooms with condoms and pads—but after she steps outside to dump the trash, she comes back looking grim. “Guess who’s here?” she calls through the sliding plexiglass window into the reception area. Biggs’s face falls. The protesters don’t usually come on Mondays, but one of their regulars is setting up across the street. Biggs texts the clinic-defender group chat to see if anyone’s available to shepherd patients to and from their appointments, then returns to her paperwork. About half of the clinic’s patients get financial assistance from abortion funds, so Briggs needs to calculate what each of today’s appointments should cost.
Some of these patients are Virginians, but many will come from surrounding areas: east Tennessee, the coalfields of West Virginia and Kentucky—places with some of the nation’s strictest abortion laws. Some drive in from Georgia, whose six-week ban is easy to overshoot, others from Alabama, where—with narrow exceptions—abortion isn’t legal at all. In October, a woman drove 11 hours from Louisiana to end her pregnancy in Bristol. Otherwise, she may have had to travel hours farther to Richmond, Charlotte, DC, or southern Illinois. “I think about people coming from that swath of red where it’s not legal,” Rosenwinge says, “and you can kind of see where they would go.”
Patients who reach Virginia may believe it’s a safe haven—a state where abortion remains legal. But even here, access is fraught. Currently, the Bristol City Council is weighing a local antiabortion ordinance, an unusual maneuver that would not have been possible under Roe. Plus, a nearby district attorney has spooked doctors with talk of the potential for prosecutions, and the clinic’s landlords are trying to drive them out. Beyond that lies a looming existential threat: If Republicans take control of state government this fall, they could try to ban abortion outright. The situation in Bristol mirrors the reality nationwide, that post-Roe, the laws and geography of abortion are still unsettled. It’s going to take years to unwind.
When the phone rings again, Rosenwinge grabs it. “Listen, no worries,” she says, “I will put it on your chart that we have to get you in and out, but I’m not going to make promises, so you should find backup for your kids.” Her voice grows conspiratorial. “Just be careful. Don’t get a speeding ticket. There’s a police officer that sits right down here, off this exit.” She explains how to dodge the trap.

The patient is driving in from a nearby state where abortion is banned. When she arrives, she’ll pull off the highway, past the new casino and a soon-to-open cannabis shop, and into the parking lot of a low-slung brick building next to a hillside of single-family homes. Outside, she’ll see a small huddle of protesters, one atop a ladder shouting through a bullhorn about murder and God. Clinic defenders in neon vests will flock to her car, surrounding her with umbrellas to protect her anonymity. Then she’ll pop through the vestibule at Bristol Women’s Health, where the staff will help her end her pregnancy, sending her back—she hopes—in time to pick up her kids from school.
Bristol Women’s Health is the brainchild of Wesley Adams, a 75-year-old ob-gyn who began practicing in Bristol, Tennessee, in 1978. Before his retirement in November, his clinic offered the full suite of gynecological care: Pap smears, fertility treatments, hormone therapy, birth control. He delivered babies—some of whom later became his gynecology patients—and also provided abortions. “If someone wanted to get pregnant, we could help them,” he says. “And if they didn’t want to be pregnant, we could help them, too.”
In Bristol, Adams says he saw about 30,000 patients, maybe 15 percent for abortions. The circumstances were mostly quotidian: financial struggles, infidelity, bad timing. But some were horrific—patients raped by their husbands, children ten or 11 years old. Adams would see girls whose abortions let them finish high school and grandmothers shocked by pregnancies they’d thought were menopause. In a few dozen cases, Adams helped place babies for adoption—if a patient was too far along or couldn’t make the decision, he’d connect the expectant mother with an adoptive family and an attorney, and they’d hash the rest out from there.
If someone wanted to get pregnant, we could help them. And if they didn’t want to be pregnant, we could help them, too.
Years ago, Krystal Biggs would drive past Adams’s clinic on her way to work as a daycare aide, horrified by the scrum of protesters outside. “I thought all I could do about it was rant on social media,” she says. Then in 2018—a few days after learning she was pregnant with her second child—Biggs noticed a cluster of pink pro-choice vests in the clinic parking lot. “So I fly down to the dollar store,” she says. “I get the flimsiest posterboard and the crappiest markers that have probably been on the shelf for two years at this point, and I haul it back up there and pull into the parking lot. I get my posterboard and my markers out, and I write, ‘A Mother by Choice, for Choice.’ ” The defenders welcomed her and gave her a vest. Biggs loved it. She began to volunteer.
For a while, Biggs stood outside the clinic every Monday, Wednesday, and Friday, sheltering patients from protesters. During that time, abortion was under assault from an additional source. In 2020, the Tennessee state legislature barred patients from seeking abortions based on the fetus’s sex, race, or genetic anomalies. Then came the 48-hour waiting period between mandatory patient counseling and an abortion, which burdened patients traveling from farther away. The legislature also mandated that any tissue from surgical abortions be cremated or buried by a funeral home, ballooning the procedure’s cost. Such laws went into and out of effect as they wound through the courts, but to Adams, the endgame seemed clear: “To make abortion illegal in Tennessee. That’s where all this was going.”
Adams considers abortion access to be paramount. “It’s just a basic right,” he says. “I mean, condoms break, birth-control pills only work [most] of the time, and having a baby is life-changing. Nobody should be made to have a child.” But it struck him that to continue providing this care, he might need to move his clinic across the state line. So in 2021, he applied for a Virginia medical license. Then, in search of a business partner, he called an old friend: Diane Derzis, the Alabama-based owner of 11 dogs, four abortion clinics, and one RV.
“I’m an activist, a feminist, a businesswoman, and I think I’m a humanitarian, but I would imagine that’s going to be heavily disputed. The overriding thing is that if a woman cannot decide when or whether to have a child, she cannot make any decisions in her life.”
Derzis didn’t need much convincing; she’s now the owner of Bristol Women’s Health. Sometimes, she’ll load the dogs into the RV and travel between her clinics in Georgia, New Mexico, and Virginia. Until recently, Jackson, Mississippi, was on that list, too—but her clinic there, Jackson Women’s Health Organization, had to close in August. That clinic was the plaintiff in a lawsuit that went all the way to the Supreme Court. The clinic lost. It was the decision that overturned Roe v. Wade.
As the clinic defenders head to Bristol Women’s Health, the air is just a notch above freezing and the clouds are beginning to break. Across the street, Samantha Cooper is ready to protest alongside two of her school-age sons. The boys sit in lawn chairs, bundled in dark hoodies and boots, while Cooper paces with a GoPro strapped to her chest. Waiting for patients, she politely explains that women who have uncoerced abortions should be executed. “I think God does not like unequal weights and measures and he calls this murder,” she says. “The Bible says a life for a life, so I do believe in capital punishment.”

Right in Cooper’s sightline is a hot-pink vinyl banner that hangs from the side of the clinic. “Honored to Be Bristol’s One and Only Officially Designated Abortion Clinic,” it reads—the words “one,” “only,” and “abortion” underlined for emphasis. “It’s wicked,” Cooper says of the sign. “It just shows how depraved this place is and how proud and boastful they are that they murder.” That banner is pure Diane Derzis: loud, brash, taking no prisoners.
Derzis is a pistol of a woman, late sixties with crackling energy, hardened from decades of abortion work. “I’m an activist, a feminist, a businesswoman, and I think I’m a humanitarian, but I would imagine that’s going to be heavily disputed,” she says by phone from Alabama, her voice a loping drawl. “The overriding thing is that if a woman cannot decide when or whether to have a child, she cannot make any decisions in her life.”
Derzis came to this work by having an abortion herself. “I got married at 19, pregnant at 20, and I was certainly in no position to have a child,” she says. This was around 1974, and “there weren’t clinics then, but there was a doctor in town who had done them for years: $125, you pulled your dress up and got on the table, then you left. Not the best experience in the world, but I got a safe abortion.”
Around that time, a Long Island housewife named Ellen McCormack launched a pro-life presidential bid. “There were fetuses all over the TV,” Derzis recalls, “and I was just energized. I was aggravated. Actually, I was incensed.” When an abortion clinic opened in Birmingham a year or so later, Derzis “bugged them to death” until they hired her as a counselor. “Then I met the women and saw those different situations they were in and I was captivated. I’d found my calling. That was it.”
The Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization was a blow to Derzis, but she’s not in the habit of backing down. In the ’90s, an antiabortion extremist bombed a clinic she owned in Birmingham, killing a security guard and maiming a nurse. Defiant, Derzis kept opening clinics, and that’s also what she’s doing now—particularly in border regions, where restrictive states meet less restrictive ones.
The politics of this can be brutal. Bristol is a conservative town known for its NASCAR track and country-music history. In 2020, Trump carried the Tennessee side by about 50 points, and the Virginia side by not much less. Last July, when Bristol Women’s Health appeared, many residents took offense—the Dobbs decision was expected to close clinics, not open them. Local churches and right-to-life groups distributed flyers and organized citizens to flood the mayor’s office with complaints.
Under pressure from their church, the building’s pro-life landlords tried to drive Derzis out—most recently by suing to end the lease. They claim their connection to the clinic has caused them “great mental anguish” and “humiliation within their business and social circles.” Their lawsuit also alleges that the lease is fraudulent, since Bristol Women’s Health identified itself as a “medical clinic” and didn’t disclose that it planned to provide abortions. Derzis and Adams laugh this off. “They took our money and they never asked us anything else,” Adams says. “If they’d Googled my name, or Diane’s name, the computer would have smoked.” The clinic’s lawyer contends that the landlords’ “regrets about the deal they made” and their “lack of due diligence” aren’t grounds to break a valid contract—but the matter remains unresolved.
Another issue arose in October, when a member of Bristol’s all-male city council introduced a zoning ordinance meant to restrict abortion; it would bar the town’s land and buildings from “caus[ing] the death or termination of a pre-born human life.” Due to state and local grandfathering laws, Bristol Women’s Health will remain open regardless, but the measure would prevent new clinics from moving in. It’s not clear if a court would uphold such an ordinance—abortion is generally considered a state issue, not a local one. But Virginia localities have fairly broad zoning powers. If this law is passed and upheld, it could become a blueprint for localities to restrict abortion nationwide.
After the zoning news broke, Derzis called the clinic and Rosenwinge answered. “Me and her were talking, and I was like, ‘Well, doesn’t that mean we’re kinda like Bristol’s only abortion clinic?’ ” Rosenwinge says, joking that by restricting other clinics, the city council was backhandedly blessing theirs. She says she could “hear the wheels turning” before Derzis replied, “Yeah, we’re kind of officially designated.” Derzis gave Rosenwinge her credit-card number and asked her to rush-order a banner, the hot-pink one that now hangs on the clinic facing the road. “If it makes one person think, or if it makes one person laugh, it was worth it,” Derzis says. “It might be a sick sense of humor, but it’s mine.”
From their folding chairs, Samantha Cooper and her sons watch a man inflate a giant Santa on the lawn of his small brick house. Cooper is seated at the edge of a parking lot across the street, as close to the clinic’s property as she can get. “Abortion Is Murder and Everybody Knows It,” says one enormous black-and-yellow sign propped against the fence. Another reads, “The Wages of Sin Is Death.”
While Rosenwinge waits for the clinic defenders to arrive, she assembles patient-care bags, hefty purple sacks stuffed with heating pads, condoms, maxi-pads, pregnancy tests, ibuprofen, and big plush socks. “I think about a woman who’s cramping, who’s having, like, the worst period of her life, and I would want to be snuggled up with some fuzzy socks and have some heating pads and just try to be as comfortable as I can.” In each bag, Rosenwinge also includes a pamphlet titled “You Are a Good Woman,” plus a small message of affirmation that she personally signs.
Rosenwinge makes these bags in a back room of the clinic, across from the break room that she’s brightened with fresh flowers—the day-old ones from Kroger, which she scoops up at a discount whenever she can. None of this is really her job—she was hired to answer phones—but she loves this clinic. She has donated artwork from her home, blankets from her late father’s hospital stays, and—most important—the framed receipt that hangs in the waiting room, dated January 27, 1973. It’s from the abortion that saved her mother’s life, five days after the Supreme Court decided Roe.
Rosenwinge’s mother, who is now 76, says she walked into the doctor’s office with a bruised face and broken teeth, suspecting she was pregnant. When the doctor confirmed it, she broke down crying—she believed that if she had this baby, her abusive husband would kill her. The doctor put his head down on the desk, then left the room and returned with a referral slip for an abortion clinic in DC.
“I think about my mother telling that little old country doctor, ‘If I have this baby, I will die,’ and him thinking enough of her to come back with that phone number,” Rosenwinge says. When she’s setting up appointments, her mom is sometimes on her mind. “When I go home at night, I know that I’ve done the right thing by a person. I know why I was born.”

After Roe fell, setting up appointments was supposed to be a scramble. Shifting state laws shuttered dozens of clinics, and the ones that remained braced for a flood of patients who could no longer get abortions in their states. This hasn’t been much of an issue in Bristol—mostly, Derzis believes, because people are ordering abortion pills by mail.
Bristol Women’s Health also offers these pills—in fact, the clinic mostly provides medication abortions, for pregnancies up to 11 weeks. It’s a two-dose regimen, and patients take their first one inside a conference room with eggshell walls and dark wood trim, surrounded by posters of female anatomy. A nurse practitioner calls in from Richmond on her lunch break, instructing the day’s patients via Zoom: The first pill stops the pregnancy from growing, then another set—taken a day or two later—expels the contents of the uterus. When the nurse practitioner is done, the patients take their first pills together. Once, Biggs saw women clinking their paper cups.
For the second set of pills, patients don’t return to the clinic—in most places, they just take them at home. But in Bristol, there’s a catch: To get a medication abortion, patients have to sign a form agreeing to take the second dose within the state of Virginia. Derzis says that’s due to Barry Staubus, the district attorney just over the state line in Tennessee.
Last summer, Staubus suggested that he might be able to prosecute doctors if a patient finishes their abortion in his state—say, by taking the first dose of their medication abortion at Bristol Women’s Health, then taking their second back home in Tennessee. (“Whether or not to prosecute would depend on the facts, on a case-by-case basis,” Staubus says.) If he ever does charge a doctor, it’s not clear he’ll win a conviction; a judge might think the abortion took place in Virginia, where the first pill was consumed. But with a felony charge at stake, doctors are on edge.
This is the reason Dr. Adams doesn’t practice at Bristol Women’s Health as he’d planned. The feedback from his lawyers was fairly unanimous: Providing abortions there would be perilous, given the unsettled legal landscape post-Roe. One concern was medical complications, which are rare in abortions but do occur. The closest hospital is just over the line in Tennessee—but Adams says he couldn’t treat a complication there, “because then you’re doing an abortion in Tennessee, which is a felony.” The closest Virginia hospital is 20 miles up the road, which would probably be fine. But at that hospital, another doctor would have to treat his patient—and Adams doesn’t know how receptive they’d be.
“Thirty years ago, I might have done it anyway,” Adams says of practicing at Bristol Women’s Health. “But at this stage of my life, it’s just not worth the risk.” He calls his quasi-forced retirement “devastating.” “I don’t like to be told what to do by somebody that doesn’t even know anything about it. I totally resent it. It’s all religion and power.”
Replacing Adams has been Derzis’s “biggest difficulty.” She says that multiple doctors have refused to practice at Bristol Women’s Health due to “the fear that has been leveled by the authorities,” a problem she hasn’t faced at her clinics in other states. “Even though our patients sign a form that states they will remain in Virginia to take their second dose,” Derzis says, “even then that’s not enough.”
Multiple doctors have refused to practice at Bristol Women’s Health due to “the fear that has been leveled by the authorities,” a problem Diane Derzis hasn’t faced at clinics in other states.
The clinic has patched its doctor hole in part with telemedicine—the nurse practitioner who calls in for medication abortions—but surgical abortions require someone onsite. A doctor from Richmond used to come down, and one from Memphis flies in from time to time. A provider in Bethesda has expressed interest, as have some medical students from North Carolina. For now, Derzis is still recruiting, and she understands why Bristol is a tough sell. “If I were a physician who put all those years into getting a medical degree, maybe I wouldn’t be likely to put that on the line.”
Whenever there’s downtime at the clinic—when patients aren’t there and paperwork is sorted—the staff sits at a cluster of desks behind the reception window, drinking mini-Sprites and talking over one another. Besieged by the protesters, the landlords, the city council, the national political climate, and their private struggles, they’ve developed a bunker mentality: gallows humor, nicknames for particularly nettlesome protesters (“rabies,” “paint chips”), war stories from clinic-defending that involve big trucks, lawsuits, and guns.
On a Friday night, they sit around past 5, then everyone but Rosenwinge trickles out. She’s about to take down the banner—“Gotta get the sign in, because you know [someone] would steal it”—when she stops herself in the entryway. There, she explains why she comes in on days off, donates heating pads and socks, spouts pro-abortion statistics at strangers at Walmart—why this cause has possessed her. She’s liberal because of her family, generations of coal miners who “stood on picket lines to stand up for themselves and their fellow man.” But she traces her activism to something that happened in the ’90s, while she was serving in the Gulf War.
“I’m driving an 18-wheeler full of jet fuel in this convoy in the middle of the night,” she says. “We’re moving towards the Tigris-Euphrates basin to hot-refuel choppers, and the guy in the truck with me decided he just—you know, he was just going to take it.” The man sexually assaulted her. “He rips my shirt off, and you know, it just—it was awful.”
Rosenwinge’s husband was deployed in the same unit, and when the convoy reached his site, she escaped the truck. “My platoon sergeants pull up and they’re like, ‘What’s going on? What’s wrong with your shirt?’ ” Still in shock, Rosenwinge explained the situation, and the sergeants went to find her husband. “They basically told him, ‘Listen, we will hold him while you hit him.’ That was their solution.”
When she got out of the army, Rosenwinge drifted through the years: jobs at truck stops, drug addiction, spans of unemployment. “I felt so untethered to this world,” she says, “because I had these strong beliefs, but no way to vent this energy that I had about my frustration with being a woman and my frustration with being told that I was only as valuable as one punch for my husband.” It felt heaviest around her young daughter. “You see this child, this innocent little girl. And you think about the things that have happened to you—about men telling you to sit down, be quiet. Or if you are outspoken like me, that you’re crazy.”
This story spills into a different one, an incident from a few nights before: At a local government meeting, while citizens debated a “pro-life county” resolution, a man tried to silence Rosenwinge. “He looks at me and goes, ‘Oh, my God—why don’t you just shut up?’ ” she says. Then he put his finger to his lips, shushing her. Rosenwinge kept her cool; she didn’t want to get thrown out of the meeting. “But I’m so angry at myself that I let that slide,” she says. “I’m not going to get violent, but you’re going to hear my opinion.”
As she tells these stories, Rosenwinge is shouting—her voice bouncing around the entryway, against the dark windows—and she stops to apologize. “I have no idea how loud I am sometimes, because when you hot-refuel helicopters, it’s very loud.” She says she can’t hear so well these days—as if that’s the reason she’s shouting while describing, over and over, the experience of not being heard.
On Monday at 10:15, the first patient is almost due to arrive. The care bags are assembled, the leaky fountain is unplugged, and there’s a pitcher of water in the conference room, ready for patients to take their pills. Rosenwinge eyes the clock, then reaches to adjust Biggs’s pin, a delicate gold uterus with pearl ovaries. The uterus has flipped upside down, which happens a lot. At home, Biggs has trained her young daughters to right it.
As Rosenwinge walks the corridor at the spine of the clinic, she envisions its future: evening and Saturday hours for folks who can’t make workday appointments, plus cosmetic improvements to make the place “homey”—rugs, cabinets, artwork for the walls, and maybe a plant for the bathrooms. “I never want patients to walk in here and feel like this is such a depressing place,” she says. “I just want them to be like, ‘Oh, I was right at home,’ and to know we took care of them.”

Outside, the clinic defenders have arrived, a half dozen volunteers with neon vests and rainbow umbrellas. One of them steps inside. “I brought you provisions,” she says, handing Biggs an expandable paper dispenser to replace the broken one at the foot of surgical table two. They discuss a patient, scheduled for later in the week, who doesn’t want the protesters to see her. The defender plans to pick her up from a nearby location and deliver her straight to the clinic door.
Perched atop a ladder, Samantha Cooper has begun shouting through her bullhorn: “Please don’t go in there today. Ma’am, there’s never a reason to murder your child. Show mercy on your child today. Your child is fearfully and wonderfully made in the image of God.” A clinic defender crosses the road, holding an enormous cardboard sign to block Cooper’s view of the day’s first patient, who is just pulling into the lot. Rosenwinge peeks outside. “Sammi’s still out there screaming like a scalded cat,” she announces, chipper as can be.
Rosenwinge can take these daily indignities: the shouting of Scripture, the zoning ordinance, the district attorney, men shushing her for speaking her mind. “I look at my little granddaughter,” she says, “who pretends to braid my hair as she’s tying it in knots, and I think: She deserves to be able to get abortion services if something happened to her. Or for whatever reason—it’s no one’s business. She should have the same opportunities that I had as a young woman.”
As the patient approaches the clinic, cocooned in umbrellas, Rosenwinge is ready to greet her. “I never dreamed that Roe v. Wade would fall and we’d be in the fight of our lives for our daughters and granddaughters,” she says, “but I’m more alive now than I’ve ever been. We’re flying by the seat of our pants literally every day, but it’s what you do—we just figure it out.”
This article appears in the February 2023 issue of Washingtonian.