On a recent autumn evening, by a golf course at the Greenbrier resort, I sipped a rye Manhattan to try to trip my heart into an arrhythmia. Scout’s honor, this was for legitimate medical reasons, though not quite in line with the doctor’s advice.
For seven-plus years, I’ve sporadically awakened in the night with my heart bludgeoning the walls of my chest. These are not panic attacks—they’re cardiac episodes, always triggered by drinking, sometimes severe enough to think I might die. A few years ago, when I confessed this to a doctor, she referred me to a cardiologist. I never followed up. It seemed complicated to work out the insurance. More to the point, I didn’t want to know.
But that morning, at the Greenbrier’s medical clinic, a heart monitor had been affixed to my chest. The nurse swabbed my skin with alcohol, then slapped it on, an hourglass-shaped device the size of a soup spoon, angled below my collarbone toward my ribs. To me, the next step was self-evident: I needed to get myself drunk in its presence. The doctor, for the record, disagreed. But if I didn’t get drunk—on top-shelf liquor, in the warm embrace of a luxury West Virginia hotel—then how could we possibly figure out what was wrong?

I’d come to the Greenbrier on assignment, to learn how the other half lives. I figured it would be like Dirty Dancing, and basically it was: quaint ballrooms and formal dinners. A man singing Sinatra in the lobby. Resplendent mountain views. The resort offers leisure galore—falconry, trout fishing, an infinity pool, carriage rides—but the activity I’d come to try was the “executive health exam.”
A two-day comprehensive physical, the executive health exam is ordinarily the preserve of elites. For $3,500—not billable to insurance—you get a battery of tests, plus substantive face time with a doctor, who evaluates your overall health. The majority of top hospitals offer these exams, alongside many clinics, spas, and resorts. Corporate employers are the main customers—fancy physicals are nice perks for executives—but private individuals sometimes buy them, too. (The Greenbrier comped mine.) If you ask a doctor, the goal is early detection of health issues. If you ask me, the goal is learning if you might imminently die.
That’s how I wound up at the golf club, 31 years young with a cardiac monitor tucked beneath my shirt. It was late September, a chill under the wind, a peach sunset glowing behind the dark spines of distant mountains. Anxious, I sipped my liquor—a poison that promised to flush my heart out of its hole, whip it into a panic, and leave it flailing around my rib cage for several lonely hours of the night. I dreaded that. But maybe the monitor would find nothing. Maybe I was the picture of health.

The week I booked my executive physical, Kim Kardashian was in the news. She’d Instagrammed about getting a $2,500 full-body MRI scan that promised to detect budding cancers, and the medical community went berserk. It’s bad preventive medicine, various doctors told the media. These scans can cause real harm.
The criticism is this: When you start poking around a presumably healthy person, you’re going to find abnormalities. Probably, they’re benign—things that never would have become problems, that didn’t need to be known. But once an issue is identified, people feel compelled to follow up. They get tests—sometimes harmful ones involving radiation—that cost significant time and money, drain hospital resources, and usually amount to nothing in the end.
View this post on Instagram
An executive health exam is not an MRI body scan, but the critique is basically the same: that it’s bad to run unnecessary tests. In a standard physical exam, care is tailored to the patient’s risks—lung screenings for certain types of smokers, colonoscopies for adults over 45. But executive health exams, critics say, run tests for the sake of running them, without regard to a patient’s actual needs. Sometimes, these exams catch issues early. But more frequently, they scare people who aren’t ill.
“Executive Physicals—Bad Medicine on Three Counts” is the title of a scathing 2008 opinion piece in the New England Journal of Medicine that I read before my trip. The author, a physician from Minnesota, blasts executive physicals as elitist and points out that their outcomes aren’t necessarily better than a standard physical exam. The article calls executive health “a whimsical extravagance that satisfies certain people’s need for exclusivity” and “almost a parody of . . . high-cost, lowreturn procedures.” It concludes that these exams are inequitable and ineffective, “a perfect example of what American medicine should be working to expunge.”
The night before my exam, cocooned in a toothpaste-colored Greenbrier suite, I contemplated the possible outcomes. The worst-case scenario was obvious: that I’d exacerbate inequities in the American healthcare system by participating in an exclusionary form of care, while simultaneously learning that I’m dying. In the best-case scenario, I’d receive an excellent physical—the kind that helps the richest Americans live, on average, ten to 15 years longer than the poor.
But the likeliest scenario, I feared, was that I’d undergo two days of testing and come out with a list of possible health concerns that—while probably nothing—might also be cancer. There would be increased 2 AM scrolling of WebMD. I already felt the dread.

My exam began with bloodwork, four dark vials sucked from a vein in my arm. Then I met with the doctor, who took the most thorough health history of my life. She was a young woman with long auburn hair. It fell across her lab coat in waves.
“Do you have a primary-care doctor?” she asked, and I cringed as I confessed that I don’t. For about an hour, I sheepishly narrated my health concerns, via charming anecdotes like these: Once, a doctor found a gallbladder polyp and told me I should keep track of it, but I never went back. And: A cash-only gynecologist once swabbed for a uterine issue and told me to call in two weeks. By the time I did, four months later, her practice had closed.

The doctor asked if I was up to date on a Pap smear (no), when I’d last been vaccinated for tetanus (no clue), and what I was doing to manage stress (pouring myself into work). Then we arrived at my heart, so I explained the genetic situation—valve issues on both sides, the kind that strike people down—while the doctor scribbled with furrowed brow. “We are going to follow up on this,” she said, which filled me with both terror and relief. That’s one benefit of the executive physical: Ghosting isn’t an option. These tests would be done. I was a captive inside a resort.
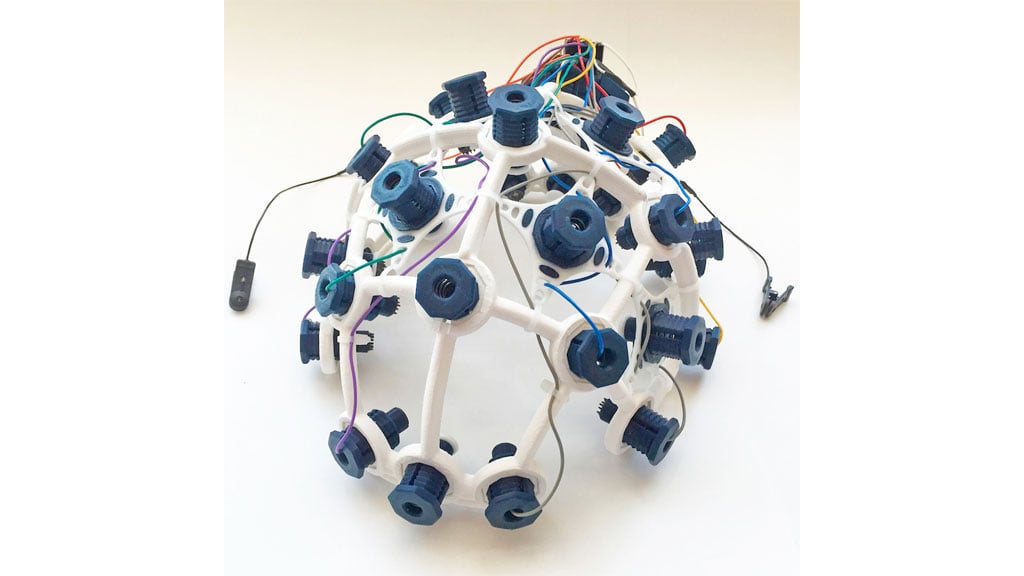
In fact, the testing commenced posthaste. Through a side door of her office, the doctor led me to a small exam room, where a nurse had prepared an EKG. “This measures the electrical workings of the heart, as opposed to the plumbing part,” she explained as she strapped 12 electrodes to my chest. Atop the same table, the doctor did a quick Pap smear. While at it, she stuck a finger up my butt, checking for something called “fecal occult blood.”
From there, I changed rooms. In the semi-dark, a sonographer slathered me with gel for an abdominal ultrasound, followed by an echocardiogram and imaging of my carotid artery. Afterward, I had a chest x-ray, then lunch: two small chicken-salad sandwiches packaged in a blue-and-green striped box, eaten in the coffee room while Antony Blinken discussed a hostage release on Fox News.
By this point, I was an hour ahead of my itinerary, but the nurse still saw me right away. First came my ear wash, a highlight of the day: warm, abrasive liquid pumped gently but persistently toward my brain. Then she tested my hearing, breathing, and orthostatic blood pressure. All of it was simple and nice.
Last came the heart monitor, the day’s sole point of friction. Apparently, for the two weeks I would wear it, I needed to keep a special phone within 30 feet of me at all times. As the nurse laid this out, I blanched. Lugging around two phones for 14 days? How would I remember, and would I look weird with a strange object adhered to my boob, and what if the phone lost charge, and what if I’m really sick? What I actually asked was “Do you see a lot of heart monitors on younger patients?” “We’ve had several,” she replied, her face revealing nothing at all.
Since I was years overdue for a tetanus shot, she offered to give me one right there. I asked to push it to tomorrow. In a couple of hours, I was headed to the Greenbrier’s gun club for skeet shooting. I needed my arms to be spry.

In response to my photographs of the Greenbrier, here is what friends have said: “It’s like Barbie lived at Graceland instead of Elvis,” and “It’s like Norman Rockwell and Tucker Carlson collaborated on a tarot deck,” and “It’s faux neoclassical mixed with Memphis mixed with rococo,” and “I like it. It’s really exciting.” All of these strike me as correct.
Leaving the clinic, I hopped on an elevator that spat me into an eddy of hotel-room doors, none of which happened to be mine. When I tried another floor, I got lost, wandering a bewildering zone of ballrooms and grand staircases and cascading chandeliers. It was a fabulous place to be trapped. The decor was delirious—carpets and wallpapers in pinks, greens, blood reds, and blacks, arranged into florals, stark geometries, and abstract designs. Finally, I confessed to an employee that I was lost. “That’s okay,” he replied. “It’s only a 1.1 million–square-foot building that isn’t symmetrical.” Then he led me down some hallways toward my room.

That afternoon, I had no obligations at the clinic—just skeet shooting and a plan to drink myself into medical distress, which commenced at the golf-course bar. Over the next several hours, I would migrate to the upper lobby, where, surrounded by dark mahogany and framed drawings of long-dead Presidents, a suited bartender shook me a gimlet. Learning of my predicament, he reassured me that his heart has a hole in it, but he’s still here.
Alone at the Greenbrier, I passed the evening texting various factoids to my friends. These messages concerned my health, the textiles, the retired congressional nuclear bunker buried beneath a wing of the hotel, and the sweet gun-club attendant who called me “ma’am” the whole time I shot clays. But primarily, the texts were about Babydog, the rotund English bulldog that belongs to the Greenbrier’s owner, West Virginia governor Jim Justice. Among her achievements, Babydog was the star of the state’s underperforming Covid-vaccine campaign (called “Do It For Babydog”), and she allegedly predicted the outcome of Super Bowl LV.
While I texted at the bar, an email from the Greenbrier Clinic popped up on my phone. My fate had arrived: Some of the test results were in. Immediately, I deleted it. To wipe my brain, I grabbed a diabolical concoction called a “lemon haze”—Hennessy, tequila, limoncello, and Cointreau—and wandered onto the balcony into the night. There, in a rocking chair around a tabletop fire, I listened to a drunk man who claimed to be an ex-cop describe the scene of a notorious Charlottesville murder. Then I got into bed, fell asleep, and woke at 4 AM with a splitting headache and racing heart, but not the arrhythmia I’d sought.
This was the worst possible outcome. I was tired and hungover, with no relevant data for the heart monitor. My fitness assessment was scheduled for 9 AM.

Returning to the clinic, I felt nervous. Somewhere inside, behind a baby-blue door, my test results awaited review. Throughout my fitness and nutrition consults, the 11 AM discharge meeting loomed. When the hour came, I marched somberly to the doctor’s office, suppressing the stray impulse to flee.

We began with my bloodwork, which actually looked fine. I’m not anemic, my glucose is normal, my cholesterol is excellent, and my kidneys work well. I was deficient in B12, but the doctor promised to give me a shot before I left. My hearing and breathing were good, and the chest x-ray found nothing substantial. Then we arrived at the locus of my dread.
The heart stuff was anticlimactic; the doctor didn’t have much news. The tests that came back looked “reassuring,” but the most telling one—the monitor—wouldn’t be reviewed until I’d worn it and mailed it back. Ordinarily, I’d have dwelled in dissatisfaction. But I was distracted. The abdominal ultrasound seemed bad.
Alarming yellow highlights marbled the printout of results; these were the doctor’s areas of concern. First were the gallbladder polyps—not one but two. In the majority of people, these are benign, she said. But they could become cancerous. I would need to monitor them to see if they grew.
Then came the “lesion on my spleen.” On the paper, beneath a highlighted streak, I saw a word that ended in “oma.” Oh God, I thought. That’s bad. In the dark pantheon of omas—sarcomas, melanomas, lymphomas, carcinomas—I knew of none that I wanted to have. Whatever a “hemangioma” was, it was probably how I would die.
The doctor, however, thought otherwise. While the ultrasound couldn’t precisely diagnose it, the spleen lesion was probably fine, akin to a birthmark or a mole. “If that’s what it is, it’s not anything we should worry about,” she said. “But we should follow it.” I swallowed hard.
I should have been prepared for that moment, since it was precisely what the critics had said; executive health exams often catch things that aren’t bothersome, that are probably benign but possibly deadly, and therefore beget pointless worry and additional care. I tried, briefly, to feel indignant. But were the lesion to turn cancerous, I’d be positioned to detect it early. I was sort of grateful to know.
At the end of my exam, the doctor pronounced me “very healthy,” and rationally I knew this was true. Still, the splenic “oma” ran skittery around my brain. I thought about it as I exited the clinic and entered an unnaturally pink restaurant for a fried-green-tomato sandwich. And that’s when I returned to my heart. It was the arrhythmia, if anything, that would kill me—although at least I was addressing it now. I’d submitted to copious testing. The monitor sat in judgment atop my chest.
By far, the executive health exam had been the best medical experience of my life. No doctor had ever spent so much time with me. No clinic had ever felt so warm. And the testing—for all its naysayers—seemed pretty targeted to my concerns. Had I gotten this care in the real world, it would have involved three or four visits to various far-flung locales, all on separate days. I would never have done it. I’d have just sat at home worrying about my heart.
Now, having tasted upscale preventive medicine, I didn’t want to go back. I dreaded a future of bleak fluorescent clinics and chaotic strip-mall urgent-cares. Couldn’t I receive all of my healthcare at a florid and maximalist resort, surrounded by foggy mountains while golfing and dining and shopping and shooting clays? Of course you loved the executive health exam, responded the cynical region of my brain. It’s a luxury product that you can’t regularly have, that most people could never afford.
But the goat cheese on my sandwich was so creamy and I was eager for my afternoon hike, where the sun would dribble over the wildflowers and the mountain air would be crisp. My nagging conscience quieted. I returned to brooding about my death.
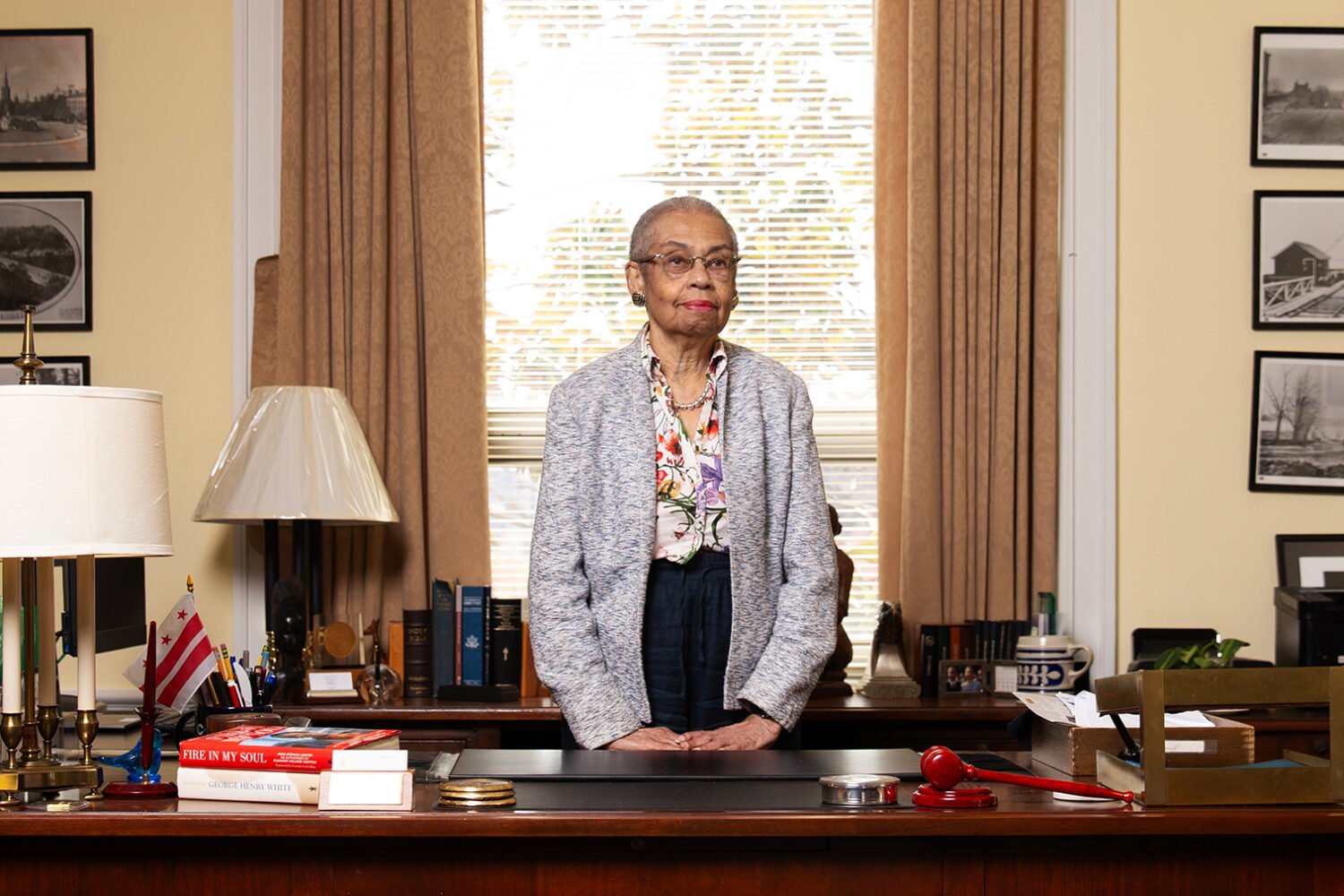
This article appears in the November 2023 issue of Washingtonian.