Breathing Lessons
"Allergies and asthma are among the leading causes of missed work or school," Dr. Howard Boltansky says. "They could be the most prevalent chronic diseases."
Boltansky, an allergist, sees a big cost for society in dollars spent on treatment for allergies and asthma. "Even worse," he says, "is the cost to the individual of being unable to enjoy life to the fullest."
Boltansky was born in Baltimore in 1953. His father was a magazine distributor and real-estate developer; his mother and other relatives worked in those businesses.
After high school in Pikesville, Maryland, Boltansky attended Tufts University, where he graduated magna cum laude with a degree in biopsychology. He received a medical degree at the University of Maryland in 1978 and did his internship and residency there.
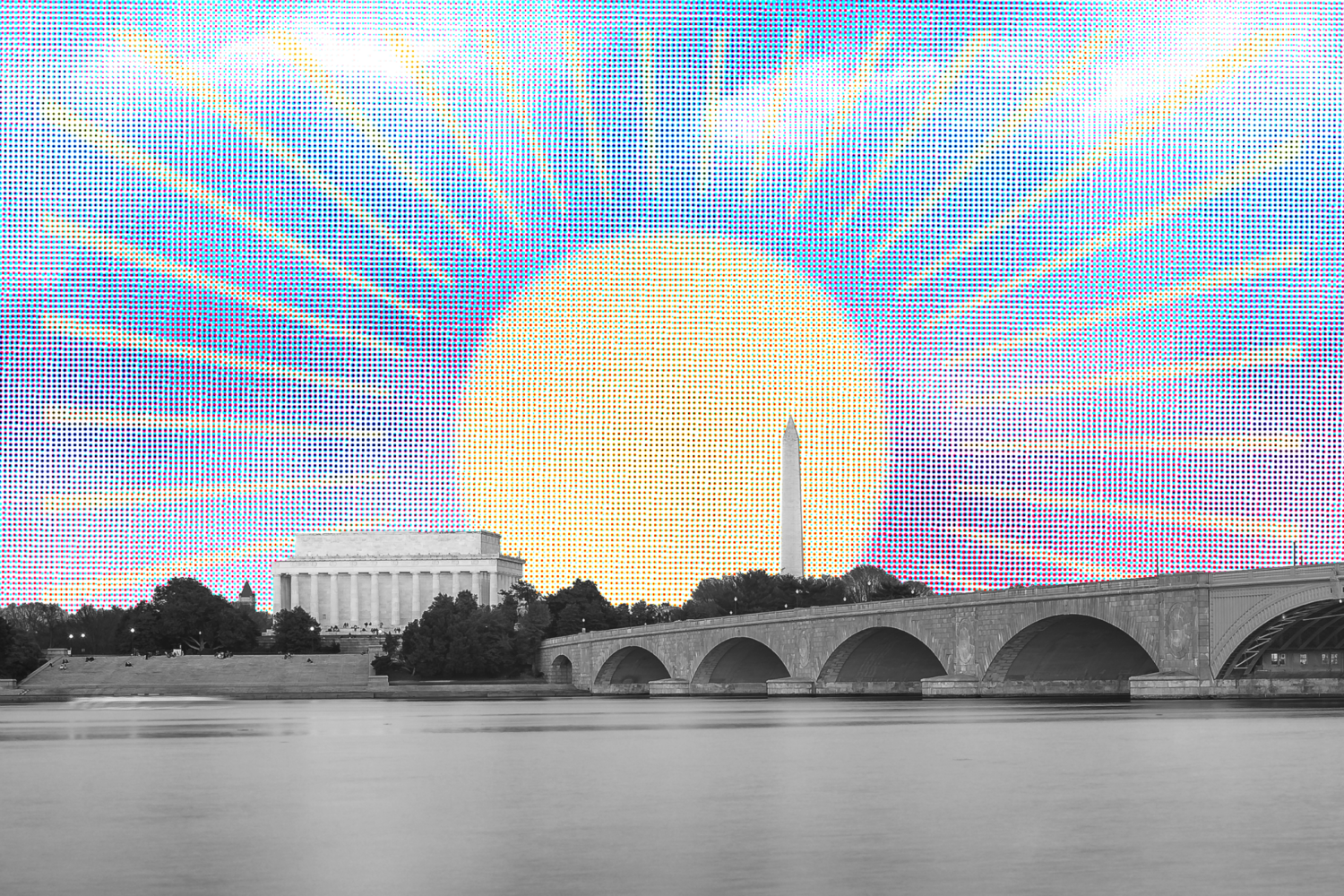
From 1982 to 1987, he was a fellow at the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. He then opened a practice in DC and Bethesda, which he still maintains. Since 1992, he has been chief of the Allergy and Immunology Section of DC's Sibley Hospital.
Boltansky lives in Chevy Chase with his wife, Merrill Lavine, a freelance museum registrar. They have four children–Isaac, a freshman at Ohio Wesleyan University; Wolf, an eighth-grader at St. Albans School; Sonya, a fifth-grader at National Presbyterian School; and Celia, a second-grader at Beauvoir school.
After an emergency consultation with a patient suffering from a severe asthma attack, we talked about what he's learned.
How bad are allergies in Washington?
Overall, Washington is a tough place for people with spring and fall pollen allergies. DC has a high rate of asthma in the inner city–especially life-threatening allergic asthma. That's partly because too many of our inner-city kids aren't connected to primary-care physicians, allergists, or pulmonary doctors.
I'm involved with IMPACT DC, a Children's Hospital program run by Dr. Stephen Teach, which identifies high-risk kids with asthma so they can get the care necessary to decrease their hospitalizations.
What's the difference between asthma and allergies?
Allergies are an immunologic condition. The body reacts to an element in the environment in an inappropriate fashion. Asthma can be allergically driven or not. Many people with asthma have no allergies.
Asthma makes breathing difficult because of inflammation, which brings rawness along the lining of the lung tubes. It then causes more mucus to be produced, which clogs the air tubes. Finally, there's a spasm of the lung tissue–muscles around the tubes–which reduces the person's ability to move air in and out.
Patients with asthma cough, wheeze, and have shortness of breath. Often there's an ache in their chest. This makes it very scary.
Between one-fifth and one-fourth of Americans have some type of allergy–Washington has a slightly higher proportion per population. But treatment for these ailments has gotten excellent. I constantly see asthmatic patients who can be helped to live full and active lives.
You don't hear of many people dying from asthma.
But they do. In the inner city particularly, asthma deaths have climbed. There are hundreds each year. Most of these people weren't on preventive medication.
The sooner we can diagnose asthma in children and the more aggressively we treat the inflammation, the better the child feels and the less lung damage is done.
Allowing asthma to go without treatment leads to irreversible changes. Patients who haven't been treated for years may have only half or two-thirds of their lung capacity. That's an enormous handicap. My job is to get the best lung function with the fewest side effects.
What causes allergies?
Genes largely determine the likelihood of allergies or asthma. If both your parents are allergic, there's a 75-percent chance you'll be. It may not be asthma, like them, or even being allergic to the same thing. But you'll have some sort of allergy. If one parent is allergic, you'll have a 40-percent chance. If neither, it's between 10 and 15 percent.
Here's what happens: Someone with allergies produces an antibody called immunoglobulin E–or IgE. It's made by certain white blood cells and attaches itself to mast cells, which are present throughout the body. These mast cells are most common in the eyes, nose, throat, skin, lungs, and the lining of the gastrointestinal tract.
When exposed to a cause of allergy such as ragweed, the IgE opens up the mast cells. Out comes histamine, which causes inflammation. In the eyes, it's allergic conjunctivitis. In the nose, it's allergic rhinitis, also called hay fever. In the lungs, it's asthma. In the skin, it's hives.
The most severe allergy is anaphylaxis, a sudden triggering of many mast cells, which release their chemicals all at once. This happens when an allergic person is stung by a bee or given intravenous penicillin or eats a lot of food he's allergic to. Suddenly, the body gets flooded with allergic chemicals. This can lead to a closing of the throat, a precipitous drop in blood pressure, an allergic shock, even death.
Someone with such severe allergies must be educated about the condition and get guidance on what to avoid. Many patients need auto-injectable adrenaline. A product called an EpiPen can be life-saving. When administered during a severe reaction, it can stabilize the body so the person can make it to the emergency room.
How seasonal are these ailments?
In Washington, we enter the tree and grass season in March and April. We finish the spring pollen season in May and June. Pollen counts during the spring are the highest of any season around here.
When counts rise between 50 and 100, many patients become sensitive. During the last few years, we've had counts as high as 2,500. Then even patients who aren't allergic get affected.
Things quiet down from July until mid- or late August. Then ragweed season opens. Ragweed pollen counts remain high until the first frost.
Patients allergic to mold cope with it year-round, as do those allergic to dust or animals. These allergies seem worse in the winter, when the heat is on, doors and windows are closed, and we're indoors more.
What's interesting about Washington is how many people who've recently moved here weren't allergic before they came. But by their second or third year–having been exposed to pollen in the spring or fall a few times–they've developed enough allergies to come into our office.
Why do allergies seem worse here than, say, New York City?
Possibly because we have more grasses, weeds, and trees. Having more plants within the city makes our pollen count higher.
What's new in treatment?
The mainstay of treatment boils down to prevention, medication, and immunotherapy–or modification of the immune system.
Prevention entails helping people understand what they should avoid, based on test results.
Medications have improved dramatically over the past 20 years. Now almost all of our patients with allergic rhinitis or conjunctivitis can be treated. They take non-sedating antihistamines, which won't generally impair their performance or sleep. Nasal-spray steroids, which cut down nasal allergies, have a great safety record. Most eye drops are fine for long-term use.
Treating asthma has also changed. Our understanding of asthma's inflammatory mechanisms led to the development of inhaled spray steroids. They don't carry the level of risk of oral steroids. These–often combined with long-acting dilator medications, which relax the air tube–reduce both the symptoms and the risks of side effects from the other medications. Our hope is that they also improve lung function.
Medications such as Singulair and Accolate–called leukotriene antagonists–have entered the market over the last few years. They reduce asthmatics' symptoms and need for other medications.
Allergy shots are still a very important treatment for patients who are highly reactive to allergens. Shots have a tremendous safety record. When a patient is identified correctly, shots have an 85-to-90-percent chance of success–significantly improving the patient's health and reducing the need for other medications. There are shots for trees and grasses, weeds, ragweed, molds, dogs, cats, and bee stings but none for foods.
Two years ago, a new injectable treatment called Xolair was approved to modify the immune system in a different way. It binds up the IgE, the allergy antibody. This treatment is the forerunner of many promising immunologic approaches to allergies and asthma in the future.
So this is an area of medicine with vast improvements?
Yes. We understand so much more about allergies and asthma than when I graduated from medical school–especially their root causes. The advances are so dramatic that anyone with allergies or asthma can now live an almost symptom-free life, with minimum side effects from medications. Granted, some people's allergies are tougher to control, but their numbers and troubles are coming down.
Take my patients who were on oral steroids to control their asthma. We used to have many who absolutely needed them. Now I have virtually no one regularly on oral steroids. And we can almost always keep people out of the hospital.
Do allergies and asthma change over one's lifetime?
Most people with a genetic tendency will have allergies or asthma during childhood. Many people outgrow these allergies, probably during hormonal changes in the immune system during puberty. Some relapse in their twenties, thirties, and forties, when they have a second wave of allergies.
A number of patients won't show symptoms until their thirties, forties, fifties–even their seventies or eighties. We've had patients without allergies their whole lives until they underwent a severe medical illness, change in hormonal status, or chemotherapy or radiation for cancer.
Why am I allergic to cats?
You weren't born with that specific allergy, but you were born with a tendency to become allergic to cats. You were exposed to cats at a sensitive time in your immune system, and thus your body made IgE antibodies against cats.
Aren't antibodies supposed to protect me?
These aren't the type of antibodies that heal us. They're different from antibodies that emerge when we get a tetanus shot or polio booster. These antibodies do us harm. We don't know why they exist.
Why does childhood asthma seem more prevalent than in the past?
The recognition of asthma in children is better today because of increased awareness and education. The actual incidence of childhood asthma definitely increased from 1980 until the late 1990s. Over the past five years, different surveillance techniques have suggested that the rate of increase has slowed or even leveled off. However, there is still a huge number of children with asthma.
What should people with allergies do to clean up their homes?
Reduce dust-collecting items, especially in the bedroom, since you spend so much time there. No stuffed animals or elaborate drapery. Get rid of old carpets, and encase pillows and mattress with dust-mite-proof materials.
A lot of people like to get high-efficiency particulate air filters, known as HEPA filters. These are portable plug-in devices that filter the air and clean out offending agents.
Keep air conditioning going in warm weather, and make sure its filters are clean. It helps somewhat to keep the humidity low in the house. Clean up all mold.
A lot of this applies to the workplace as well. If your allergies are worse at work, ask the building management to check its air-conditioning filters and to look for mold.
The carpet in your office may be old and full of mold and dust mites. If so, it should be changed. Maybe you sit next to a colleague who wears an irritant perfume. Check that out, too.
What are general allergy do's and don'ts for living in Washington?
Don't accept that your allergy or asthma will limit you in any major physical way. Treatment nowadays is so excellent that a doctor can get you back doing whatever you love to do.
Take medications as prescribed. That's the only way we can evaluate their effectiveness.
Every asthmatic patient should have a peak-flow meter. This hand-held device monitors lung function at home, and it's pretty cheap. Checking every day shows whether you're beginning to slide down that slippery slope of asthma.
Very few people get quick asthma attacks–ones that become dramatic in hours. Usually people begin to slide days ahead of a crisis. Had they monitored their peak-flow meter, they would have known to seek medical care. We've found the peak-flow meter to be among the best tools to prevent major asthmatic exacerbations or deaths.
If you're highly allergic to a bee sting, don't walk barefoot through grassy fields, drink from open soda cans, or have a picnic near open food containers that attract bees.
Keep your EpiPen handy. It does you no good having it back home.
Be especially vigilant about children with allergies, especially food allergies. Make sure everyone in that child's life knows what must be avoided. Keep an EpiPen near the child and know how to use it.
If you could pick two areas in need of medical breakthroughs, what would they be?
First, for my asthmatic patients, the development of an anti-inflammatory medication like an inhaled steroid, one free of long-term side effects. Medications being developed are a step forward, but we aren't there yet. There's still a risk of side effects over the long term.
Second, in the emerging field of pharmacogenetics I hope it will be possible in the future to test the blood or saliva of allergic patients and asthmatics to determine which medications would work best. This would remove much of the guesswork.
Further off would be genetic engineering, to turn off a person's asthma or allergies. I hope to live to see this done for patients who really need it.
Overall, what have you learned about asthma and allergies?
I've learned that the most important part of a patient's visit is the personal history. It's then that I connect with the patient, earn his or her trust, and learn the nature of the problem.
I've learned that treatments available in my field are constantly becoming more effective and safer. We need to do a better job of making sure all patients with these diseases have access to them.
What have you learned about life?
That what really matters is our relationships. Being there for the people we love is the essence of life. Life flies by so quickly, but those moments when we form a bond with someone, when we laugh or cry with them, are the moments we can hold onto forever.
We all have an obligation to help others.