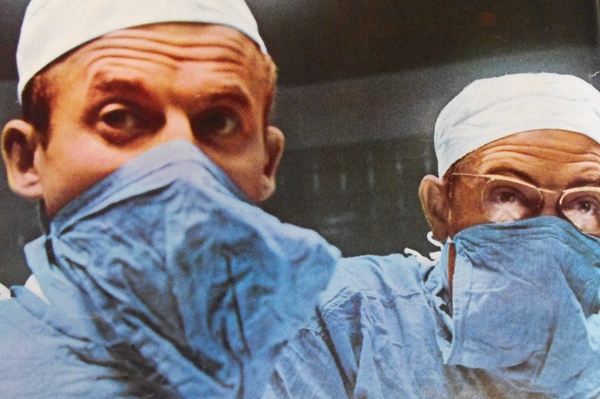
A survey conducted by the American College of Surgeons found that surgeons have a higher drinking rate than the rest of the US population. Photograph courtesy of Flickr user libertygrace0.
We already know Americans—Washingtonians in particular—like to drink. But it turns out that surgeons tend to hit the bottle even more than the rest of us.
A recent survey released by the Archives of Surgery found that the rate of alcohol abuse among US surgeons—15 percent—is higher than the general public’s rate, which hovers around 6 to 8 percent, according to the National Institute on Alcohol Abuse and Alcoholism.
The survey, conducted by the American College of Surgeons, asked more than 25,000 surgeons about their drinking habits. Out of the 7,197 surgeons who answered, 15 percent scored in the range of alcohol abuse and dependence, based off the Alcohol Use Disorders Identification Test.
Dr. John Ricotta, chair of surgery at MedStar Washington Hospital Center, is surprised by the high number, but he is well aware that it is an issue among surgeons. “Surgeons have a tough and very demanding lifestyle. It doesn’t surprise me that there’s a significant problem with substance abuse.”
The survey also found that female surgeons’ alcohol abuse rate was double that of males’, at 26 percent. Surgeons who reported being “burned out” or depressed also increased their chances of alcohol dependence.
While the study did not explain why the female rate was significantly higher, Ricotta, who was not involved with the study, says it probably has to do with the culture of the medical field, though balancing work and life is becoming easier.
“Surgery is a difficult career for everybody. I think it would be fair to say that for many women who went into surgery more than ten years ago, they had to make a very conscious effort to unbalance their work and lifestyle,” he explains. “At some point, that’s probably going to manifest as discontent and depression.” And that, he adds, eventually may lead to alcohol abuse and dependence.
Also disturbing is that surgeons who reported a major medical error in the past three months were more likely to have a drinking problem. However, Ricotta says the chances of a surgeon going into surgery while under the influence are extremely low. “I’ve been in active practice for 30 years, and I can’t think of more than one or two circumstances where I’ve seen a physician incapacitated,” he says. “In each of those cases, the physician was immediately sequestered.”
In cases where a surgeon’s substance abuse problem is known, Ricotta says there is a pathway for him or her to deal with it. Typically, the medical license is either restricted or the physician is pulled from medical services. Once that happens, Ricotta says that the pathway to treatment needs to provide a non-punitive atmosphere, so that the physicians get appropriate disclosure.
“To solve the problem and salvage the careers of people who have spent 20 to 25 years training for something, you have to have a pathway open to these individuals that will be nonstigmatizing,” he says.
The good news from this survey is that the findings do not represent the majority of all US surgeons. Factors associated with a lower likelihood of alcohol abuse or dependency included being male, having children, or working for the Department of Veterans Affairs .
The results will likely provide an increased incentive to address not just patients’ well-being, but physicians’, too. “We understand that both burnout and dependency are major issues we’re going to have to identify, study, and address,” Ricotta explains.
“The bad part is on one hand, we found out we’re not perfect,” he says. “The good part? We sort of knew we weren’t perfect, and now we’re learning how to deal with it.”
To read an abstract of the study, click here.