Al Newland engineered his own health-care reform a little more than a year ago. His son, Martin, then 13, was sick for several days with fever and stomach pain. The family’s doctor in Vienna waved off the symptoms, but Martin grew weaker and unable to hold down food.
Four days after the trip to the doctor, Newland took his son to the emergency room at Inova Fairfax, where the underlying problem was diagnosed: Martin’s appendix had burst. The complications were serious enough that the teenager was hospitalized twice and lost 40 pounds. For more than two months, he took antibiotics intravenously every six hours.
With that, Newland left the Vienna practice—“They treated you like a number,” he says—and on a friend’s recommendation signed up himself, his son, and his wife, Nancy Heaney, with PartnerMD, a company based in Richmond that had opened a McLean practice.
PartnerMD is the latest entry in “concierge medicine,” a primary-care model that is booming as dysfunction within America’s health-care system grows. Patients in a concierge practice typically pay an annual retainer or membership fee of $1,500 to $3,000. Doctors in turn reduce their patient load—from as many as 3,000 to typically about 600—and promise same-day appointments, 24/7 access to physicians, and lots of preventive screening.
The payoff for the doctor can be attractive: A $1,500 retainer for a practice of 600 grosses $900,000. “That’s serious money before you even say hello to a patient,” says Peter Lavine, an orthopedic surgeon and president of the Medical Society of DC. For patients, the arrangement also can be very attractive. No more cooling your heels in crowded waiting rooms. No more hurried consultations with a doctor who can’t remember your name.
Some worry that concierge care sharpens the divide between the haves and the have-nots. But the model is cheered by others as the seed of a health-care revolution.
Concierge care debuted in Seattle in 1996 and has captured the interest of a relatively small number of doctors. The Society for Innovative Medical Practice Design, a seven-year-old association promoting the model, estimates 5,000 doctors are in concierge medicine nationwide.
No one tracks data on concierge doctors in the Washington area. John Richards, executive director of the Medical Society of Northern Virginia, says the model got attention here a few years ago and estimates that there are now a couple of hundred concierge practitioners areawide.
MDVIP, a national concierge company that opened in 2000, counts Washington as one of its best markets. More than 30 of its 330-plus doctors work in the area; many of the physicians closed up traditional practices and reopened under the MDVIP banner. Their patients typically received a letter and an offer to help them find a new doctor if they didn’t enroll in the new practice.
There’s nothing radical about the idea that profit can be made from an enhanced patient/doctor relationship. More than 60 years ago, the Greenbrier in West Virginia opened an “executive health” clinic with extensive physicals, preventive screening, and a bit of pampering. Johns Hopkins and the Mayo and Cleveland clinics have similar programs that are the gold standard today, offering everything from electrocardiograms to a complete blood chemistry. Such programs operate locally, including at Inova Fairfax Hospital and Virginia Hospital Center.
Executive physicals, however, tend to be one-shot deals: You meet with a doctor, undergo a battery of tests, then return to the care of your regular physician. Concierge care typically offers a version of that physical, but the physician conducting the tests becomes your doctor.
PartnerMD was founded by Richmond entrepreneur Linda Nash. Like Al Newland, Nash had a beef with her doctor. In Montana on vacation, she was thrown from a horse and taken to the hospital. Her husband and the hospital tried repeatedly to reach her family physician in Virginia. “A doctor’s staff can be as dogged as gatekeepers,” Nash says. “It’s all about keeping consumers away to maximize the physician’s time.”
From that experience, Nash saw a business opportunity. In 2003, she opened PartnerMD with one doctor and about 40 patients. The practice has grown to 3,500 patients and nine doctors, and the company projects 10-percent growth in revenues in 2009.
PartnerMD patients pay $1,900 a year in membership fees, with a $1,500 charge for spouses and $600 per child. Otherwise, the company’s practices operate very much like traditional fee-for-service doctors, negotiating rates with insurance companies and charging patients accordingly. Membership includes an annual physical, but patients still pay deductibles and copays.
Nearly two years ago, PartnerMD expanded to McLean, aiming to tap business executives in the Tysons Corner area and families with two harried professionals.
PartnerMD’s offices on the seventh floor of a downtown McLean building are well appointed but not lavish. During several visits, the waiting room often was empty, devoid of disgruntled people whose appointments were scheduled to have started an hour ago.
To open the office, PartnerMD hired Sandy Ibrahim, a young family doctor married to a Comcast engineer. The daughter of Egyptian immigrants, Ibrahim, 35, studied microbiology at the University of Michigan in her hometown of Ann Arbor, then went to Wayne State University’s medical school, one of the biggest producers of primary-care doctors in the country. She never considered any specialty but family medicine.
“I wanted continuity with the patient, to grow with them and become part of their family,” she says.
After finishing her residency in 2003, Ibrahim joined a practice in Fairfax, then another in McLean, but found neither satisfying. She raced through appointments and left work too exhausted to care for her two young children. As one of the younger doctors in both practices, she was expected to make room in her schedule for fevers, sore throats, stubbed toes, and other same-day emergencies.
“It was urgent-care, pump-it-out, production-line work,” she says.
With a patient load of more than 2,000, she struggled to make connections or even to remember names. Says Ibrahim: “I would grab lunch at the grocery store, bump into a patient I had seen that morning, and not remember that I saw them.”
Having decided it was time to leave clinical work, she began exploring jobs on Capitol Hill and research work at NIH and the Centers for Disease Control and Prevention. After just five years in practice, she was going to give up seeing patients and abandon a career that had been her dream.
Ibrahim’s story is not unusual. In a survey of family practitioners and general internists last year by researchers at the University of Wisconsin, about half called their work life chaotic; a quarter reported burnout. Fewer than a quarter said that their practice “strongly emphasized quality.”
Doctors blame Medicare and insurance, which offer more generous reimbursement for procedures than for the office visit, history-taking, and conversation that are critical to primary care. There’s always been a gap between reimbursement rates for specialists versus primary-care physicians, says Janice Ragland, a Herndon doctor who’s president of the Virginia Academy of Family Physicians. “That gap used to be two to one. Now it’s four to one.”
According to an annual survey by a national medical-placement firm, family doctors, pediatricians, and general internists are the lowest-paid physicians, making $171,000 to $186,000 a year. Orthopedists make nearly $500,000 a year, while radiologists take home nearly $400,000.
“There’s too much work and not enough pay,” Ragland says. “We spend probably 40 percent of our time on paperwork, phone calls, reviewing labs—work that doesn’t get reimbursed.”
Faced with low reimbursements, general practitioners often pack as many patients into a day as possible. Even then, they may put in long hours, hustling through ten-minute appointments to maintain a practice that gets by on thin margins.
Doctors in training hear these war stories and choose specialties that promise more money—particularly those physicians-to-be who’ll leave medical school in debt. In the past ten years, the number of medical-school graduates who choose residencies in family medicine has dropped by half. Numbers also have fallen, if not as dramatically, in pediatrics and general medicine.
Declining entry into primary-care medicine reflects a generational change in attitudes as well. Years ago, doctors going into practice were committed to working sunup to sundown to give patients full access, says Dr. Shyrl Sistrunk, associate dean for curriculum management at Georgetown University School of Medicine.
“That’s really not a model being propagated now,” Sistrunk says. Med-school students are interested in a career with flexibility so they can take time off for children, relief work abroad, or other ventures.
“Rarely does a student talk about the money they want to make,” Sistrunk says. “They talk about the lifestyle they want.”
The declining number of young primary-care doctors couldn’t come at a worse time. General practitioners are retiring in large numbers just as waiting rooms are filling up with baby boomers who’ll need extensive medical care in the coming decades. The shortage of primary-care doctors will only be more noticeable if the health-care reform moving through Congress succeeds in giving millions more Americans access to doctors for the first time.
Sandy Ibrahim was scouting non-clinical jobs when she heard about PartnerMD. She attended one of the company’s recruiting events, where company officials and doctors mingled over cocktails. Then she went through a year of interviews and vetting, including trips to Richmond.
Ibrahim liked PartnerMD’s promise that she could spend the time with patients to practice medicine as she had been trained. She sensed that the job would translate to a better balance of her work and home life.
“Yes, I’m a doctor,” she adds. “But I’m also a mom, a wife, a sister, and a daughter. I have many other hats that I wear. Maybe it’s my generation, but being a doctor can’t be my entire identity.
“I took a pay cut to come here—a $25,000 pay cut. That’s how miserable I was.”
Nearly two years later, Ibrahim has nearly 400 patients. Though some are from her old practice, she didn’t remember some when they showed up at PartnerMD.
Each patient gets a yearly health assessment that includes bloodwork, a physical exam, and a session with a nutrition-and-fitness coach. The process takes up to three hours. At her old practice, Ibrahim says, she crammed physicals into 15 minutes.
On any day at PartnerMD, she sees eight to ten patients, about a third of her load before. “You just get to know so much more about each person,” she says. “I now have the kind of relationships with patients that probably took my former boss 15 to 20 years to make.”
The extra time allows her to focus on prevention. “Let’s say a patient comes in for a physical, and his blood-glucose level comes back at 101,” Ibrahim says. “That’s just barely prediabetic; normal is less than 100. In my old practice, we’d see how the patient did at his next physical. Or maybe we’d have him come back in six months.”
“Here, when I get a level of 101, I have the time to research that. I’ll go back and look at old records and try to pick things up in their family history, lifestyle, medications, or other factors. And I’ll tell him: ‘This is what I want you to do. I don’t want to wait until you are diabetic.’
“That’s pretty aggressive. In my old practice, we might have waited until the blood-glucose level was 120. But I don’t want to wait. We’re trying to catch those pink flags before they become red flags.”
Dr. Timothy Soncrant was also looking to do better preventive care when he opened the David Drew Clinic in the late 1990s. The founder of the clinical-treatment program at the National Institute on Aging, Soncrant created a small practice whose signature is a marathon annual physical with a battery of tests that include image screening for cancer, blocked arteries, and aortic aneurisms.
Today he and colleague Jeffrey A. Elting, a White House physician for Bill Clinton, manage the care of no more than 1,000 patients, each of whom pays about $4,000 to $5,000 a year for the physical and routine care.
Many doctors who convert to concierge medicine don’t go it alone. After more than 20 years in medicine, Bethesda internist Alan Sheff made the leap only after MDVIP, the Florida-based for-profit concierge network, evaluated his patient base to determine whether enough of them would follow him to the new venture. Company officials also helped organize several town-hall-like meetings, each with hundreds of patients, to explain the change.
“A physician who tried to do this on his or her own could really break the practice in an irreversible way,” Sheff says. He opened his doors in 2003 with about 300 patients, nearly all from his old practice of almost 3,000. He’s now capped his patient load at 550, and he has a waiting list.
MDVIP collects the $1,500 annual fee from patients and pays the physician $1,000. Sheff says he lik
es that MDVIP sets quality and service standards for its doctors; offices must be staffed to answer the phone—“By the second ring!” says Sheff—and he must give patients written reports following physicals.
“I don’t have to wear the business hat all day long,” he says. “I’m back to being a doctor.”
Mark Vasiliadis and Kevin Kelleher, longtime family doctors in Northern Virginia, opened a concierge practice in 2004 while continuing to run their traditional office. They considered MDVIP but ultimately decided that they wanted their new business, Executive Healthcare Services in Reston, to reflect their own standards of care.
“We had the sense that we would be constrained in their practice model,” Kelleher says. “Our goal was just to provide better and unique care; it wasn’t to become concierge doctors.”
Vasiliadis and Kelleher limit their patient loads to 300 patients each—about half of a typical MDVIP practice. Each pays a retainer of $200 a month, or $2,400 annually, with children at $50 a month. Nearly 100 percent of patients renew, Kelleher says.
Kelleher says they focus their practice on wellness and prevention. They see the primary-care doctor almost as a coach who motivates his patients to do the work—through diet, exercise, medication, and the like—to maintain their health and keep small problems from turning into big ones. When they need specialty care, they consult with the outside doctors and track patients’ care and progress.
Tech entrepreneur Roger Mody came to Executive Healthcare Services shortly after the new practice opened. He was 41 and had largely ignored his health—until Vasiliadis found a potentially life-threatening problem. Vasiliadis became the quarterback for managing his care; within days, the doctor had set up appointments with specialists, and surgery was arranged to head off the trouble.
“Their relationships with specialists give you immediate access,” Mody says. “You get exclusive privileges, almost like having an American Express black card.”
After the surgery, the doctors checked in with Mody frequently through e-mails and phone calls to make sure he was following his home routine for recovery. “They stayed after me,” Mody says.
Kelleher patient Bobbie Kilberg, CEO of the Northern Virginia Technology Council, says the doctor took two hours out of his day to go with her for an imaging scan she was worried about: “He has your back every step of the way, no matter how many specialists you go to.”
Critics of concierge care say it smacks of elitism. They worry that its growth will lead to a two-tiered health-care system where patients in the second tier get inferior doctors and poor care.
“Concierge care is great, but who can afford it?” says Dr. Barbara Starfield, codirector of the Johns Hopkins University Primary Care Policy Center. “It’s not a solution for the country; it’s a solution for rich people.”
Concierge advocates claim that their model of medicine is unfairly cast as something only for the rich. They say teachers, plumbers, and other middle-income workers sign up because they’ve made health a top priority.
“I hate the term ‘concierge,’ ” says Darin Engelhardt, president of MDVIP. “It connotes someone who can get tickets to a good show or a Redskins game. We like to refer to it as ‘personalized preventive care.’ At $4 a day, it’s a very viable option for many, many Americans.”
More than a few entrepreneurs are banking on the idea that concierge medicine can be done more cheaply. Privia Health, a start-up company in Alexandria, is building a network of doctors in Washington who charge monthly fees of between $25 and $75 for concierge-like guarantees of 24/7 access and care focused on prevention and wellness with the help of fitness and nutrition counselors. Unlike MDVIP or other concierge doctors, Privia physicians maintain a traditional practice and ask patients to see nurse practitioners for routine ailments.
“I don’t need a trained, experienced doctor to look in my ear and tell me I have an ear infection,” says CEO Jeff Butler.
New Atlantic Ventures, a Reston venture-capital firm, invested $1.5 million last spring in Qliance, a Seattle company that’s pioneering what it calls “direct primary care” because it eliminates insurance companies as the middleman. For a fixed price as low as $600 a year, Qliance patients get concierge-like guarantees of 24/7 access to the company’s doctors and 30-minute appointments along with free X-rays and basic lab tests. Patients need catastrophic insurance coverage, but they pay nothing beyond the retainer for their office visits and primary care.
Qliance has opened only three clinics in Washington state, but its backers believe its business model could revolutionize health care in the same way that Amazon transformed the book business. By doing away with insurance, they say, Qliance is eliminating the back-office support that’s driving up the costs of all care.
“It’s concierge medicine for the masses,” says New Atlantic founder John Backus. “We really think it is the solution to the health-care problem in America.”
If nothing else, concierge medicine offers a case study of what primary care should look like—and how it might cut costs. More-personalized care might lead to early detection and proper treatment for diabetes, heart disease, hypertension, and other chronic illnesses that untreated can explode to require expensive surgical procedures and hospital stays. MDVIP touts a study showing that its patients are admitted to the hospital much less frequently than others. Research by the David Drew Clinic shows that its preventive screening catches diseases early and lowers the death rate for patients.
It’s easy to dismiss the findings of a for-profit company that makes its services look good, but no one disputes that the concierge model of care is attractive.
“We all agree that you need to be able to really coordinate the care of your patient,” says Lori Heim, president of the American Academy of Family Physicians. “If you do that, you will have a tremendous cost saving in the future. It’s a whole lot cheaper for me to manage my diabetics than to pay for an amputation or dialysis.”
But Heim is skeptical that the concierge model could be made affordable on a widespread scale. She’s talked to many doctors—particularly in rural areas—who’ve researched the idea and find they could never make it work financially.
Heim and others see potential in other solutions. They say policy reformers have awakened to the primary-care crisis and its role in the growing costs of health care. The reform moving through Congress likely will include Medicare-reimbursement increases for primary providers as well as loan forgiveness and other measures to make general medicine more attractive to young doctors.
More promising are schemes to reinvent how health care is delivered. Today that delivery is fragmented: A middle-aged professional might see an internist, an endocrinologist, an orthopedist, and a rheumatologist or pulmonologist. Yet rarely does any single doctor adequately monitor the progress of a patient.
The health-care-reform legislation includes pilot projects to end that fragmentation by paying the general practitioner to coordinate a patient’s care. In a pilot program that loosely resembles the concierge or retainer practice, fee for service would remain the norm, but Medicare and other insurers would pay a monthly per-patient fee to physicians who treat chronically ill patients through a “medical home” model. The home would include a medical team—perhaps a nurse practitioner, a nutritionist, and others—who would emphasize preventive medicine through routine visits, screenings, and monitoring of diet, exercise, and medication. The doctor would also oversee patient visits to specialists and hospitalizations.
The medical-home concept is backed by Heim’s American Academy of Family Physicians and other doctor groups. “We understand the pressures that drive physicians and patients to the concierge model,” Heim says. The medical-home concept and payment system, she argues, could offer comparable care for more people.
Another Medicare pilot program would pay primary-care providers not through a monthly fee but through a share of savings generated by the reduced costs of care. In one such program, called Independence at Home, geriatric physicians would head teams of nurse practitioners and social workers to coordinate care for severely ill Medicare patients in their homes. Such care could head off serious complications and hospitalizations, leading to cost savings that the teams would share.
Dr. Eric De Jonge, who runs an at-home geriatrics program at Washington Hospital Center based on this model, argues that using patient outcomes to determine pay will improve care as well as reduce costs. “How do you justify paying extra money to providers when not holding them accountable for results?” De Jonge says. “We have to start paying for quality and economic results.”
In the meantime, Sandy Ibrahim continues her own version of health-care reform. Ibrahim says she practices medicine more cost-effectively now than she e
ver has. In her old practice, with only ten minutes to see each patient, she often ordered tests because she didn’t have time for a thorough evaluation. Now she can take her time and focus on prevention and wellness.
PartnerMD recently added a second doctor to its McLean practice—Donald Rhodes, who’s a solo practitioner in Centreville. That means Ibrahim’s patient load shouldn’t top 400 anytime soon.
Ibrahim resists the notion that her care is elitist. Many of her patients aren’t wealthy, she says. Some pony up for PartnerMD to get a doctor who has time to monitor a chronic illness closely—people with diabetes or heart disease or patients recovering from cancer treatment or surgeries. “They want to make sure things aren’t missed,” she says.
Ibrahim likens her move into concierge practice to the teacher who decides to work in a private school: “It’s a personal choice.”
She’s heard the argument that if more doctors go to concierge medicine, the shortage of physicians will only get worse for the average Joe. “Well, you almost lost me as a family doctor to a non-clinical job,” she says. “At the end of the day, I’m a happy practicing doctor, which I think is much more important than being a disgruntled doctor who’s not practicing medicine.”
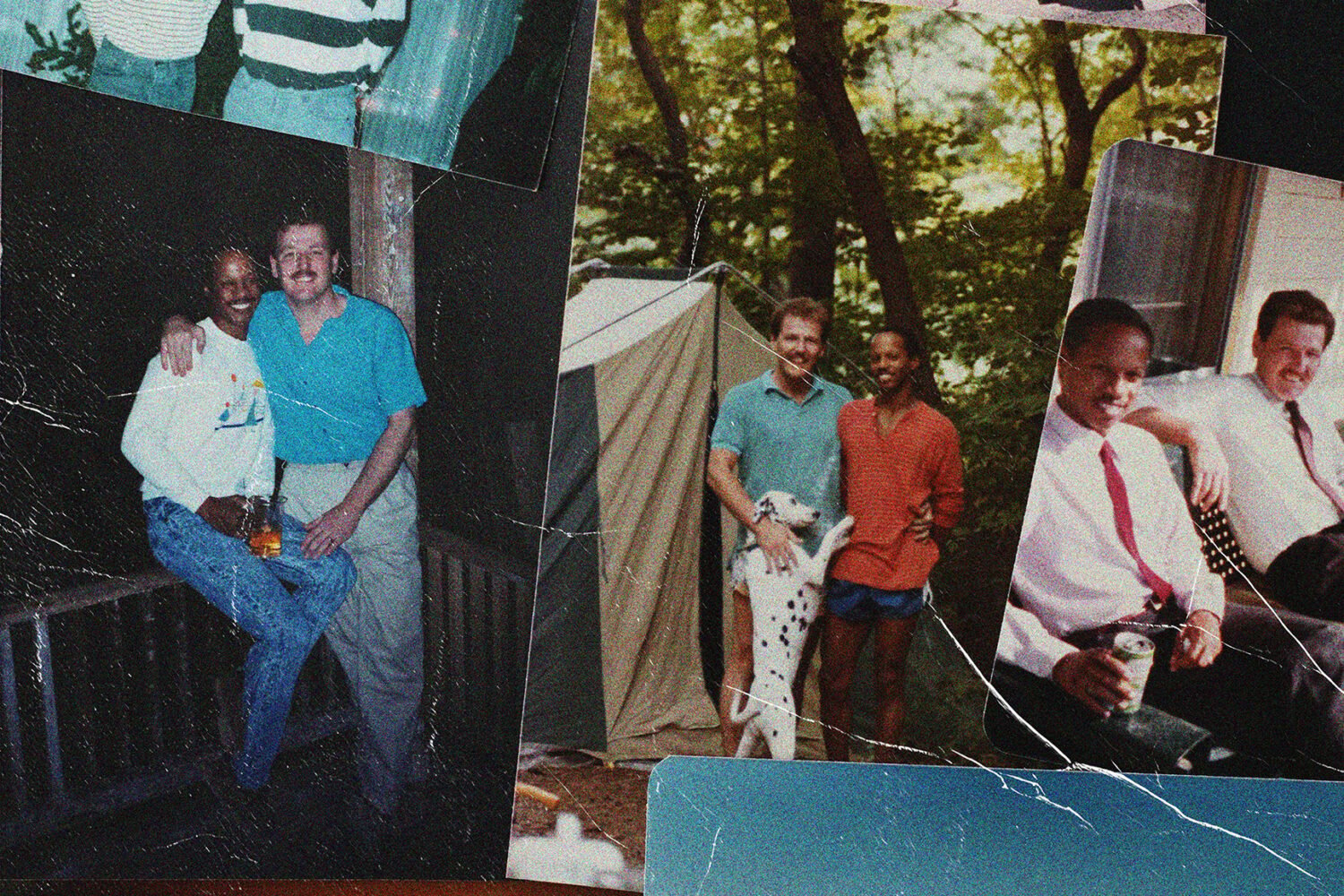
Al Newland, meanwhile, couldn’t be happier. His wife has a chronic illness that he believes Ibrahim is watching closely. His son, Martin, now a sophomore playing football and soccer at Madison High in Vienna, has broken a finger and injured his knee since the appendix episode. Each time, Newland says, Ibrahim has arranged for him to see specialists and watched over his care.
Newland is not wealthy; he and his wife are both retired 20-year Navy veterans, though he continues to work as an IT specialist for the Department of the Treasury. The PartnerMD retainer isn’t cheap, but his military insurance isn’t expensive at $450 a year. He’s willing to pay more to get better care.
Says Newland: “The peace of mind for me is worth every penny.”