National editor Ken Adelman (adelmank@aol.com) has been conducting What I've Learned interviews since 1988.
"I nag a lot," says Alice Rosenberg, who coordinates HIV/AIDS outpatient care at the National Institutes of Health's Clinical Center in Bethesda. "I start out warm and fuzzy, and then go mean and nasty."
The District has one of the nation's highest per capita incidences of HIV infection, and AIDS particularly lends itself to nursing care. "People have to be called regularly," Rosenberg says. " 'Did you take your pills today? Why didn't you?' "
Nursing those with AIDS is a skill in high demand: "Very few are standing in line for my job."
Rosenberg, 63, was born in Mamaroneck, New York. Her father was a truck driver, now deceased; her mother, a former telephone operator, is 94.
After completing her training at the Yale-New Haven Hospital in 1962, Rosenberg worked at Peter Bent Brigham Hospital in Boston. In the 1980s, she edited the Journal of Immunotherapy and taught aerobic dance at the Bethesda-Chevy Chase YMCA while raising her children. From 1995 to 1999, she was head of nursing at DC's Whitman-Walker Clinic.
She lives in Potomac with her husband, Steven, chief of surgery at NIH's National Cancer Institute. They have three children. Beth teaches high-school English in New Jersey; Rachel is practice manager for a local law firm; Naomi is a premed student.
After an emergency call on a patient, we talked about what Rosenberg has learned.
Is AIDS a chronic disease now?
It's become more of one since treatments have become so effective. Nonetheless, most people with AIDS now will die from it or its complications. The lifespan of someone with AIDS used to be 15 years after initial infection. New medicines extend this. They can extend good quality of life, but sometimes they extend the part of life with the highest occurrence of complications.
How well or how long life is extended depends on how faithfully patients take their medicine and whether they develop secondary problems. Many are also heroin addicts or alcoholics–neither of which encourages rigorous compliance. Some are infected with other diseases as well.
Is there a false sense of security because of the advances in treatment?
When AIDS medicines called protease inhibitors were first available in the mid-1990s and the initial results were so positive, yes, there was a flood of media reports that the worst was over. This led to increased-risk behavior. Many thought, "All I have to do is take some medicine and I'll be okay."
It's since been demonstrated that this medicine isn't so easy to take. It's expensive, it can be toxic, and resistance frequently occurs.
Who's getting AIDS now?
More women, for sure. When I started at Whitman-Walker in the early '90s, 7 percent of my patients were women. When I left in '99, it was 24 percent. Now it's a little higher than that.
AIDS has very much become a heterosexual illness. Heterosexuals are at risk each time they have unprotected sex with a person they don't know–and often with someone they do. The receptive partner is far more likely to get infected; a female is more likely to be infected by a male.
Many gay men are back in sex clubs. Young gay men contracting HIV weren't around for the first wave. They didn't know the 30- or 40-year-olds infected then, most of whom are dead now. And the press now hypes the treatments, which drives precautions down further.
I used to talk to high-school kids constantly. They all think they're immune. Their friends are young and healthy. And they're not particularly promiscuous. They don't understand that it doesn't take much to get infected. They're not sleeping with just one individual–they're sleeping with every person who ever slept with that individual.
A few years ago, when I toured high schools talking about AIDS, I was told not to use the word "condom." I had to say "latex product," and only when speaking of family planning.
A group called Metro TeenAIDS is now very active in doing outreach to area high schools.
Where is the incidence of AIDS rising?
The number of young gay men getting infected is approaching the levels of the mid-'80s. Besides an increased incidence among women, there's been a steep rise among minorities. This increase is partly because there are more cases and partly because there's better reporting of cases.
The statistics are tough to get accurate. Rate of incidence doesn't necessarily equal rate of treatment, as there are eight to ten years between infection and the occurrence of symptoms. Current estimates for Washington show that as many as 30 percent of people infected with HIV are unaware that they're HIV-positive.
In general, many of the people seeking treatment are males 15 to 35 years old, and they don't adhere well to treatment. They're not accustomed to complying with rules. When they do, the medicine doesn't make them feel better. They get nauseated–which isn't positive reinforcement.
But isn't it a death sentence not to take the medicines?
Sure, but that's over the long term. These people aren't thinking long term. Many have dealt with drug addiction, alcoholism, and poverty before contracting HIV. Many have lost their jobs since becoming sick. They have no money and go on welfare.
We help all of our patients follow their regimens by simple steps like giving them cab fare to go to the doctor, or childcare if they're mothers. I have a patient now–a young woman who's HIV-positive. Her child's positive, too. The mother sends the kid off to school, and the girl has diarrhea on the bus and returns home. That mother won't make it to her own doctor's appointment that day.
One of our key medications causes nightmares and vivid dreams. These patients wake up feeling like they haven't slept. So we schedule the medication better. Such adjustments take a lot of phone calls and support.
I tell patients: "Come in and see me. When you feel you want to kill yourself, just come in. Spend the day with us here. Maybe you'll feel a bit better."
I warn them that they're going to hear from me and hear from me and hear from me. One of my patients, a guy whose wife also had AIDS and died recently, told me that if he ever gets married again, he'll do so during Passover because he knows I'm gone then and won't be bothering him.
What works in prevention?
Condoms. I beg providers for cases of them. I want them readily available–hoping that if someone has them, that person will use them.
Condoms should be available in schools. Making them so doesn't create promiscuity. It's embarrassing for kids to go to the drugstore to buy condoms. We've got to accept that high-school kids have sex. Using condoms is the only real way of preventing the spread of HIV.
You have no faith in abstinence?
It's beyond naïve to think that abstinence will work. You'd be counting on kids not to do the natural thing. A small core of devout Christian kids might buy that, but not the vast majority. Certainly not college kids, who have a newfound freedom and space to have sex.
What's a common reaction when you tell young people they're HIV-positive?
Most cry. They're stunned: "I can't believe this has happened to me. How am I going to tell my family? My friends?"
I suggest, "Perhaps you should wait to tell anybody until you're used to it yourself." This gives a person a chance to feel some sense of control as well as time to determine what to say and to whom. That might take a week, sometimes a month. I say, "Get your head together first, however long that takes. And don't have unprotected sex."
After being told they're HIV-positive, some can't wait to get out the door. I won't hear from them for a month or more. They're in denial. Others say, "I just knew it was going to happen to me"–as if they had nothing to do with it.
I ask them to backtrack: "When do you think you got infected? What happened since then? You need to be in touch with those people." They have a responsibility to tell their sexual contacts. I can help with that process if necessary.
How does someone with AIDS end up at NIH's Clinical Center instead of at a local clinic like Whitman-Walker?
The center includes a 242-bed hospital with patients from around Washington. New patients hear about us by word of mouth. Another part of the Clinical Center is the much larger research clinic. It gets referrals through primary-care physicians and patients themselves who are investigating new treatment protocols on the Web. These patients come from all over the world.
Treating people with AIDS costs a lot of money.
Oh, my God, yes. Each patient costs tens of thousands a year. Each takes a combination of three to five medicines to treat AIDS, and most will require two or three more to prevent other infections or minimize the recurrence of infections. Many patients–including poor ones–get help from government programs.
We don't start any treatment until a patient's immune system has deteriorated to roughly a third of its normal capacity. According to our best information, starting treatment earlier doesn't help.
What's it like to be with people at the end of their lives?
I share a unique intimacy with someone living his or her last days on earth. Once they have their financial affairs in order, it's my job to get the family to be supportive.
Patients tell me how they want to be buried and remembered. Most have no recent pictures of themselves. When I ask for a good picture, they show me one from five or six years ago.
Many worry about having trouble breathing and being in pain. We have medicines and other ways to keep them comfortable. They come to understand they don't have to be afraid.
Some ask to hear their favorite music or a poem. If a friend stops by, they want to hear that person's voice. They ask me to position their friends outside the door, and they talk to them from there. Their bodies are wasted–down to 80 or 90 pounds–and they don't want to be remembered like that.
What do they want you to do?
Talk to them. Keep them comfortable. If they have trouble breathing, I'll get them oxygen. If they're in pain, I'll get them morphine.
Do many talk about God?
Not much. After five or eight years of battling AIDS, most talk of God is gone. A few go back to Jesus, but most feel nothing spiritual after being so sick for so long. They've lost confidence that God is looking after them.
Many choose to be cremated, since they don't want to remain the way they are. They get very involved in where their ashes go. Some have their funeral before dying. They want to hear the eulogies, to hear what people think of them.
At the very end, rarely do they resist death. Most have little strength left. They go gently.
What have you learned from helping them die?
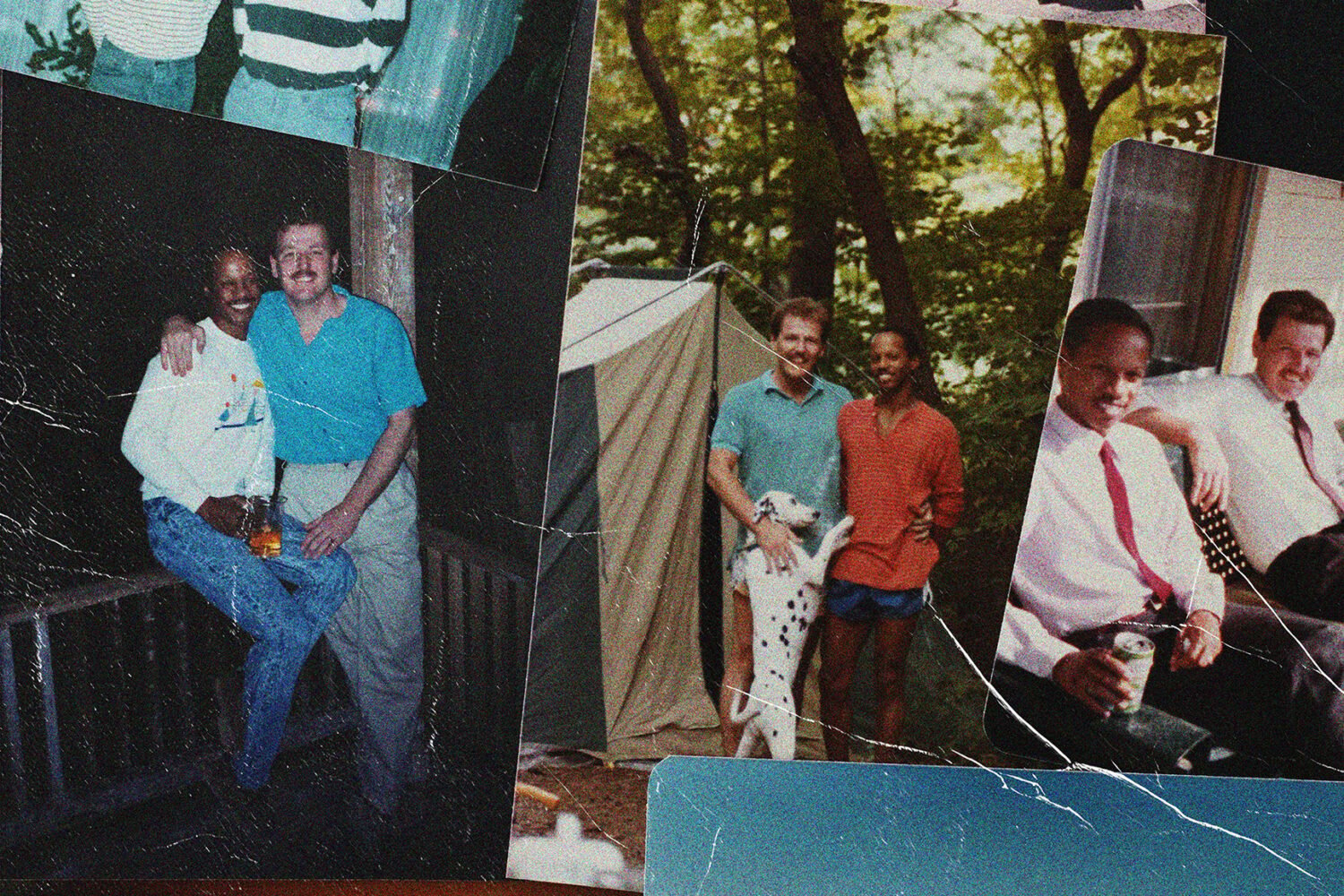
Among gay men with AIDS, it's how supportive the gay community is. When one of them gets sick, they circle the wagons. They pick the guy up, carry him to the bathroom, make sure he eats and gets what he needs. The strength and character of that community is remarkable.
I was stunned by the lack of the medical establishment's response to this illness early on. The federal government was slow to pick up on the need and offer support, but it's much better now. AIDS is now a disability, so someone contracting it becomes eligible for government support. That was a while in coming.
What have you learned about treating people with AIDS?
How clever this virus is. It mutates around everything put in its way. When we started with the drug AZT, the virus quickly went around that. We constantly need new drug combinations. We now have 23 anti-HIV medications.
There won't be a vaccine soon. Anything injected to prevent the virus from replicating will prompt the virus to go around that and replicate.
I've learned how unaccepting people are of HIV and AIDS. They don't want to hear about it. Few can accept how susceptible their children are–even good kids in Ivy League schools.
What have you learned about family reactions?
In the case of gay men, that they're mostly abysmal. I've called many parents to tell them, "Your boy is very ill. You know he's gay. Now I must tell you he has AIDS and he would like to see you."
Many respond that they won't have anything to do with him. So we end our conversation by my saying, "I'm awfully sorry, since your involvement could really help your son."
Sometimes a mother will call back months later. I'll often have to say, "Your boy is not with us anymore."
The mom then becomes weepy and remorseful. But where has she been for the past five years, when her son had no money, no help, and was asking me to care for him?
Brothers tend to have trouble with the gay thing. Sisters are much better. Sisters stick. They don't have the same baggage as parents or brothers. Often the family support comes from the sister.
Why do you do this work?
After staying home for 20 years raising children, I wanted to return to nursing–but only where I was really needed. I didn't need a swanky downtown office.
Isn't it depressing?
Not for me. It's a privilege to help people die with dignity.
What do they say?
Not much, since usually we're both crying by then.
What have you learned about life?
Do what you really want to do. And make every day count, because you don't know when it'll end. Things change very, very quickly.