“There is something about a disability that wakes us up,” says Ed Eckenhoff. “I don’t know whether we begin overcompensating or we realize we have fewer options for success. I do know it made me rethink my future, and I have observed this with a lot of people who suffered disabilities.”
Eckenhoff—who recently retired as head of National Rehabilitation Hospital—grew up in Swarthmore, Pennsylvania, where he enjoyed life as a middling student and outstanding athlete. Tall, strong, one of four brothers, he played fullback on the Swarthmore High School football team, played tennis, and captained the track team.
After high school, each of the Eckenhoff sons was encouraged to spend a year in Europe. Ed chose the University of Munich, where he studied two things he loves to this day: art and piano. He returned from Germany to enter Kentucky’s Transylvania University, the small liberal-arts school that his father—an anesthesiologist who became dean of Northwestern’s medical school and later president of Northwestern University’s medical center—had attended.
Eckenhoff played on the college tennis team and dabbled in academics. In 1963, at age 20, while he was riding in the passenger seat of his roommate’s MG, his life changed when the sports car crashed, throwing him from the vehicle. He landed on his back and was paralyzed from the waist down. His roommate died.
Eckenhoff returned to college the next year, outfitted with leg braces and crutches and transformed from a happy-go-lucky jock into a serious student who got onto what he calls the “right” dean’s list.
After graduation, still unsure of what to do with his life, he went to the University of Kentucky for a master’s in education and psychology and counseled disadvantaged children in Kentucky’s Fayette County. He then enrolled in the Washington University School of Medicine in St. Louis and earned a master’s in health-care administration. From 1974 to 1982, he worked at the Rehabilitation Institute of Chicago, where he became vice president of administration.
Seeing a need in the Washington area, in 1984 he founded National Rehabilitation Hospital, whose inpatient services are headquartered in DC. He served as president and CEO until his retirement in October at age 66.
Eckenhoff oversaw the hospital’s growth and the establishment of 40 outpatient rehabilitation sites in the area. In the years of his leadership, NRH has grown into an internationally recognized rehabilitation hospital that has admitted nearly 40,000 inpatients and had more than 2 million outpatient visits. U.S. News consistently rates it as one of America’s best hospitals.
Eckenhoff’s tenure also saw the development of a major research endeavor, the Christoph Ruesch Research Center at NRH. He helped forge an academic relationship with Georgetown University Hospital and a clinical relationship with the National Institutes of Health. He extended NRH’s research arm to develop a relationship with the military in seeking better ways to rehabilitate soldiers with major disabilities such as traumatic brain and spinal-cord injuries as well as amputations.
Eckenhoff has been a tireless advocate for the disabled. He received the Citation of a Layman for Distinguished Service, the highest award given to non-physicians by the American Medical Association.
In 2007, following the disclosure of substandard conditions at Walter Reed Army Medical Center, President Bush appointed Eckenhoff to the Commission on Care for America’s Returning Wounded Warriors, chaired by former Health and Human Services Secretary Donna Shalala and former US senator Bob Dole. The commission was charged with evaluating rehabilitation programs and services and making recommendations to improve care for injured soldiers and their families. To Eckenhoff’s disappointment, most of its recommendations have yet to be implemented.
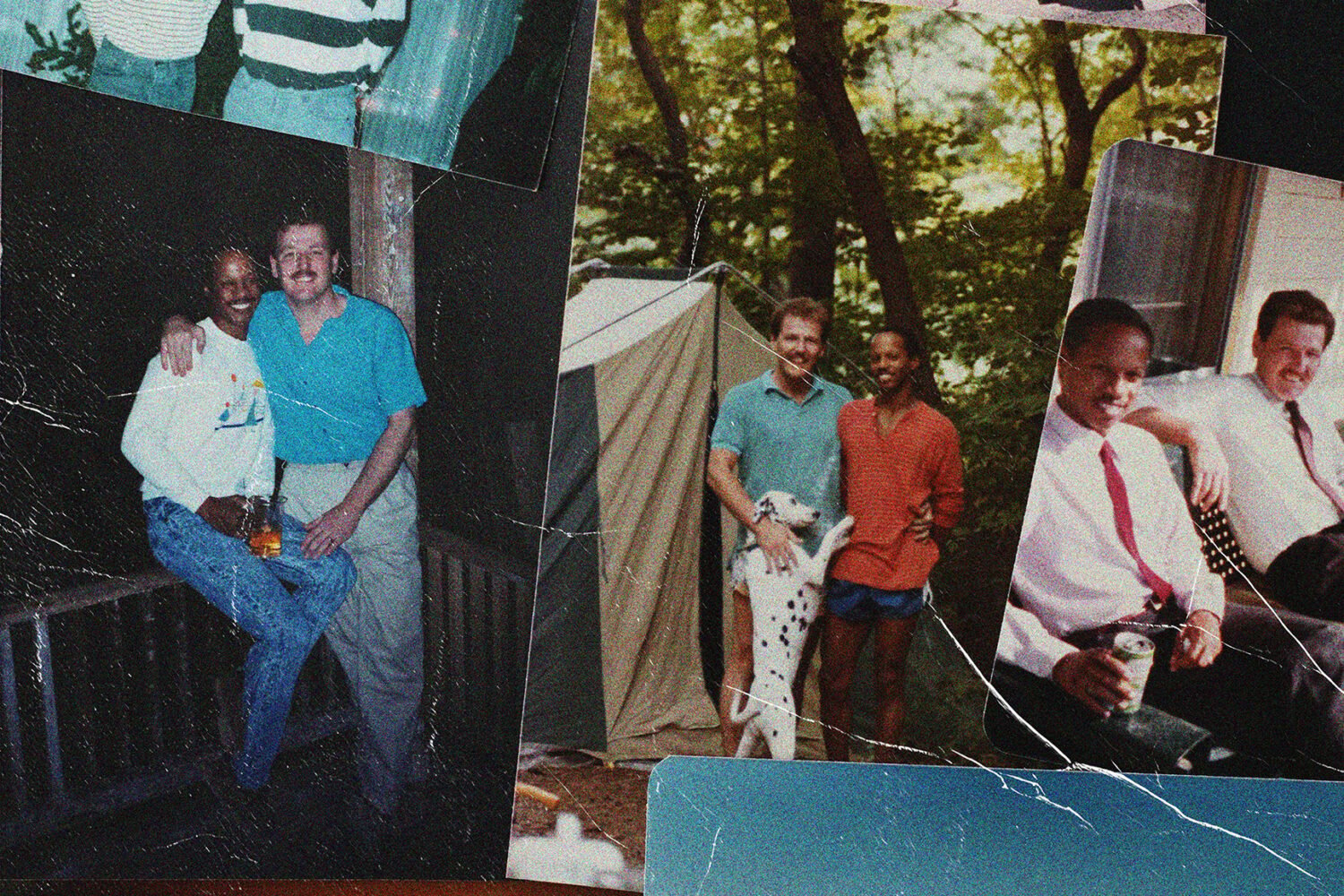
Eckenhoff lives in an apartment on DC’s Pennsylvania Avenue with his wife, Judi, whom he met in Illinois and married in 1977. Despite his disability, Eckenhoff never lost his athletic competitiveness and for years has been an avid golfer who swings with one arm and uses the other to hold his crutch and balance himself.
You seem to be saying your disability helped make you successful.
My experience and that of others have shown that many people who accept their disability have risen to greater heights than they would have if they had not had the disability. Because of how the accident changed me, I’ve led a purposeful and fulfilling life. I’m not sure this would have been true if I had not suffered my injury.
Who has been inspirational to you?
There are thousands of people. I’m on the patient floors much of the time, and I’ve gotten to know many people who’ve overcome incredible disabilities. Many of our NRH team members are disabled, and I’ve found their stories inspiring.
When I served on the Commission on Care for America’s Returning Wounded Warriors, I went to Walter Reed and met soldiers and family members. When I spoke with these soldiers who had became disabled by IED blasts, they told me they wanted to return to Iraq to serve. I found it incredibly inspiring to witness their courage.
When you had your accident, spinal-cord injuries were considered irreversible. That’s not the case now, is it?
No, thankfully it is not. We’ve made a lot of strides in the early treatment of spinal-cord injuries. We know now that giving methylprednisolone, a steroid that reduces inflammation, to someone right after a spinal injury can preserve an increased degree of function. In some cases there have been reversals of spinal-cord injuries. A player for the Buffalo Bills, Kevin Everett, had a spinal-cord injury while playing football. His spine was cooled, and he was given methylprednisolone right after the injury. He has made a remarkable recovery and is walking again.
The one area that might hold the most promise for people with spinal-cord injuries is stem-cell research. I think in time it will make an enormous difference in spinal-cord and perhaps brain injuries.
What changes have you seen for people with disabilities?
It would be a long list. But one example: When I was injured, there were no curb cuts to allow people in wheelchairs to cross streets. The same is true of access ramps and access to public transportation. Boarding a bus or airplane was virtually impossible if you were in a wheelchair. That’s one reason I chose leg braces and crutches instead of a wheelchair.
Because it was so hard for people with disabilities to get around, many were confined to their homes or institutionalized. It’s a different story today, in part because of the 1990 passage of the Americans with Disabilities Act, which allows disabled people to enjoy access to most of the same things able-bodied people enjoy.
What’s been the impact of new types of information technology?
The changes have been staggering. Cell phones, computers, and other electronic devices benefit disabled people by allowing them to maintain channels of communication in ways they never could before.
Disabled people can access a computer using voice recognition or other means. There’s a device called brain-computer interface that allows someone to communicate by thinking various commands. This device then translates those thoughts to the computer. It’s incredible how these technologies are expanding the lives of people with significant disabilities.
How about prosthetic devices?
We’ve seen the development of prosthetic arms than can be guided by the brain. Transistors are inserted into the prosthetic-robotic limb. Signals from the brain are sent to the limb. The Department of Defense is seeking to develop a prosthetic arm so advanced it can be placed on a soldier so he can return to the front line if he’s lost an arm. This was the stuff of science fiction when I was injured.
Have NRH researchers taken part in these new developments?
We were involved in some of the precursor research that led to the development of the brain-computer interface, and NRH scientists also helped develop something called “eye gaze,” in which someone can look at a computer screen and pick out letters to build words and sentences.
This high tech sounds expensive.
Yes, and unfortunately inaccessible to many. I still wear basically the same steel-and-leather braces that FDR wore 65 years ago. New braces have been made from carbon-fiber epoxy resins, the same material used in lighter wheelchairs, reducing the weight of leg braces by more than half. But if an insurer can pay $7,000 for a pair of steel braces, it won’t want to spend $10,000 for a pair of carbon-fiber epoxy-resin braces. This is the problem with any new technology. If you are a paraplegic, you either get a pair of braces like me or you get a wheelchair, but you probably can’t get both.
How are rising health-care costs affecting rehabilitation?
In many ways—most of them not good. We have a much higher level of medical and clinical sophistication than we had 20 years ago, and that adds to our cost.
Like everyone else in medicine, we’re getting hit by health insurers looking for ways to cut costs. We often negotiate with financial providers who don’t comprehend the value of rehabilitation. This is not always their fault. Many financial providers are simply so young they don’t grasp the benefits of rehabilitation following a stroke or spinal-cord injury.
Acute-rehabilitation hospitals are also getting competition from nursing homes that put “rehabilitation” in their title. That will confuse someone from Aetna or BlueCross BlueShield who is negotiating costs and discovers that rehab in a nursing home costs $600 a day while comprehensive rehabilitation at a specialty hospital runs $2,000 a day. If a nursing home gives an hour of therapy a day and we provide a minimum of three hours of rehabilitation a day, who do you think insurance companies will contract with?
Are rehabilitation hospitals an endangered species?
Any medical institution that does not pay attention to a multitude of metrics will not be able to defend its existence. If someone goes to an acute-care hospital for a procedure, he or she can either live or die. When admitted to a rehabilitation hospital, how does one measure how much better the person will live after rehabilitation? This is difficult to quantify.
That said, we’re never going to transfer people with spinal-cord or traumatic brain injuries straight from an acute-care hospital to home, so we will continue to perform a vital function. Some people, such as those with a hip or knee replacement, who don’t require high-intensity rehabilitation and don’t need to be in a rehabilitation hospital such as NRH probably can go to a less intensive rehabilitation setting. But people with serious injuries need the intensive rehab we offer, and that’s costly.
The rub will be whether someone with a major disability receives the high level of rehabilitation care that we know they require or whether these people will be referred to a less intensive rehabilitation setting because it’s cheaper. Few health insurers think long-term and consider a person’s independence and potential productivity over a lifetime.
What don’t the able-bodied get about rehabilitation?
Few people take the time to understand rehabilitation until they need it or a loved one needs it. Why learn about something when you hope you’ll never need it? A million and a half people a year in this country suffer traumatic head injuries, and maybe 100,000 of those suffer an injury serious enough to cause the permanent loss of one life function. Another 800,000 Americans suffer strokes every year, and some 10,000 young people suffer spinal-cord injuries. When you add them all up, it is still less than a million people annually, and we have 300 million living in the country. But this is changing as we live longer. More Americans are living with permanent disabilities than ever before.
What kind of health-care reform do you think we need?
I should plead the Fifth on this one. We have two basic problems in health care—cost and access. I used to think the only system that would solve the access problem would be a single payer, but I’ve seen what’s happened in the last 10 to 15 years with the English and Canadian systems, with the long waits, rationing, and denial of care, and I no longer think a single payer will solve the access problem.
I continue to believe our health-care system to be the very best in the world, and I get upset with people, including our President, who say the system is broken. It is not broken. We know of the nearly 47 million people who do not have health insurance. This is a serious problem, but you don’t have to revolutionize the health-care system to accommodate those 47 million.
Expanding Medicaid might be a way that state health-care systems could address the access issue, and by increasing federal allotments to the states these people could be picked up on Medicaid rolls. I don’t know if this is the answer, but I think by enhancing an existing part of our payment structure we could solve the access issue.
If we can solve the access issue, we can incrementally chip away at making our system more cost-effective. This makes a whole lot more sense to me than trying to overhaul the entire system at a cost of $1 trillion. And I can tell you it will become far more expensive than that.
Are people with disabilities sometimes perceived unfairly by able-bodied people?
Frequently the disabled are talked down to as people who are not only different but also not too bright. I don’t know how many times I’ve spoken to people who don’t know me and seem to think I’m wearing a brace on my brain as well as my legs. That’s one reason I’ve practiced being gregarious, because I want the first words from my mouth to show everyone that I can talk, think, and engage in conversation.
Are some people afraid to approach you?
Yes, but it’s gotten better. I remember when I used to go to the grocery store and a child would come up to me and say, “Hey, mister, what happened to you?” and the mother would pull the child away and admonish him, “Don’t ask him that question.” But all that child was trying to do was learn why I walk the way I do. Kids still come up to me, and I feel an obligation to talk to them and let them know I’m okay.
Anything you’re especially proud of?
Our NRH team members. We’ve been able to attract world-class people not only in our clinical area but in our research as well. Gathering an outstanding group of 1,000-plus team members is my greatest single accomplishment at NRH. I’m also very proud of the fact that we are one of the largest rehabilitation-research centers in the nation.
What are you planning to do in retirement?
I’m going to remain on the NRH board for the next three years, and I’ll chair long-range planning efforts. I’ll be going up to Capitol Hill to try and secure funding for all of the missions for which we don’t receive one dollar from insurers, such as research, training, and education. We want to be a model like NIH, where we will be the place that understands what to do with disability before anyone else does. I’ll be involved in the philanthropic major-gift requests. This will probably take half of my time, so I’m not cutting the proverbial umbilical cord quite yet.
I may also play a little more golf, and I’ll paint and sketch more now that I’ll have the time. My wife, Judi, and I will spend the winter in Florida, but we’ll never move from Washington because we love this city.