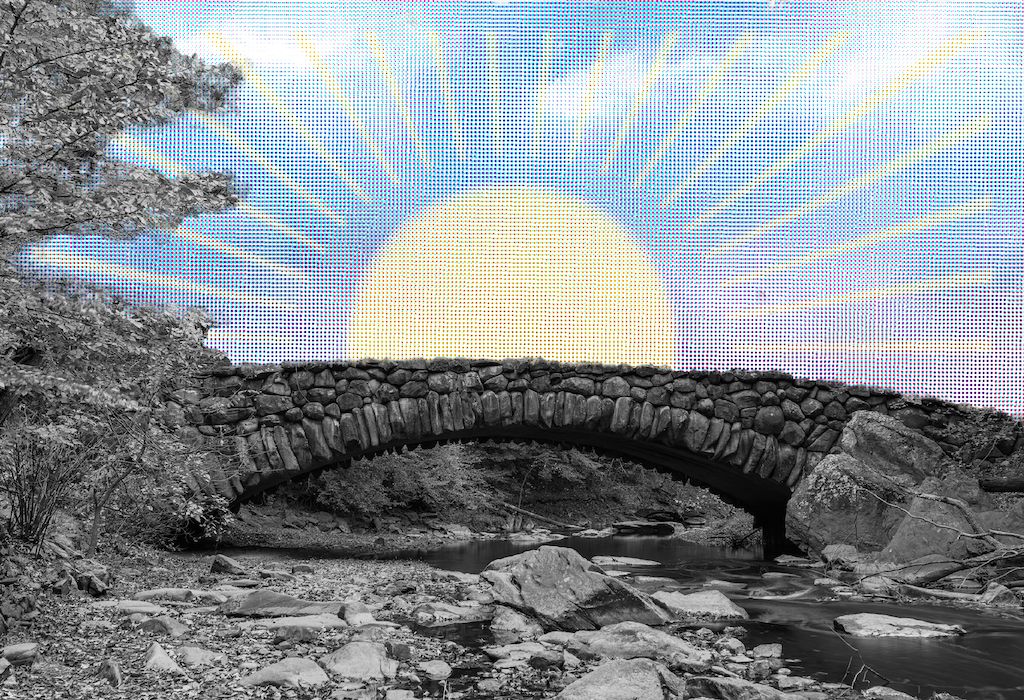
The author felt like her old self within two weeks of going off gluten.
Photograph by Mark Bennington.
It was a nurse in my internist’s office who raised the question: “This sounds like it could be gluten-related,” she said after listening to my list of ailments from rashes to stomach discomfort. “Have you considered that?”
That was two years ago. I’d barely heard of gluten intolerance, let alone the array of symptoms it was capable of triggering. All I knew was that, since returning from a vacation in Maine, I’d felt crummy. Nothing—rest, vitamins, doctors’ visits, medications—seemed to help. The old symptoms kept returning or new ones would emerge.
In the ensuing months I would undergo a battery of tests and begin my own investigation into why I felt so bad. By the end, I’d know more about gluten than many doctors. At age 48—after a lifetime of eating foods containing gluten without incident—I would be diagnosed with non-celiac gluten intolerance, also known as gluten sensitivity.
What Is Gluten?
A protein found in wheat, barley, and rye, gluten has been around a long time, though experts believe some grains may now contain more of it because of changes in the way grains are grown. Besides the obvious—breads, pretzels, beer, and pasta—many processed foods contain gluten, usually as a binder or stabilizer. Examples are salad dressings, candy, soups, baked goods, sauces, gravies, and ice cream. Or as my physician put it, “Gluten is in anything that tastes good.”
Until recently, if you’d heard of gluten, it was probably because someone you knew had celiac disease. In people with that condition, gluten triggers antibodies that attack the body’s tissues and damage intestinal villi, finger-like projections in the digestive tract that absorb nutrients. People with celiac disease commonly experience intermittent diarrhea, bloating, and abdominal pain. But there may be less obvious symptoms: depression and anxiety, muscle cramps, rashes, fatigue, anemia, joint pain, and tingling in the legs and feet.
The symptoms can be similar to those of other conditions such as Crohn’s disease, irritable bowel syndrome, and gastric ulcers, which is why, according to one study, celiac disease takes an average of four years to diagnose. The only way to treat it is to adopt a gluten-free diet. Failure to do so can lead to serious health problems, such as malnutrition, osteoporosis, infertility, certain cancers, and neurological problems.
Gluten sensitivity often mirrors celiac disease in its symptoms and sometimes in the time they take to emerge, though with gluten sensitivity the symptoms normally occur faster—often within days, compared with weeks or months for celiac disease. Gluten sensitivity is also treated by cutting out gluten.
The main difference is that gluten sensitivity isn’t an autoimmune disorder and isn’t thought to be life-threatening, says Dr. Alessio Fasano, director of the University of Maryland Center for Celiac Research and lead author of a recent study on gluten sensitivity.
“You are not going to die of gluten sensitivity,” Fasano says, “but your lifestyle can be greatly affected if it goes undiagnosed. Dealing with it can be so stressful and the symptoms so debilitating that it can cause someone to lose their job, lose their partner, things like that.”
For two months before my diagnosis, I experienced brain fog and anxiety that made focusing on work difficult. I was tired and fell into the habit of taking naps. An avid exerciser, I had whittled my workouts—on the rare occasion I felt up to one—from an hour down to ten minutes, due to muscle aches and weakness. My skin itched all the time, to the point of interfering with sleep. And my sinuses were so congested that I rarely went out.
Fasano’s study, published last year in the journal BMC Medicine, provides the first evidence of key differences between gluten sensitivity and celiac disease. Fasano says the two conditions are part of a spectrum of gluten-related disorders.
An estimated 18 million Americans, or 6 percent of the population, suffer from gluten sensitivity, according to the Center for Celiac Research, and Fasano expects the number to climb. Meanwhile, there’s been a fourfold increase in celiac disease over the past 50 years, with just under 1 percent of the population—about 2.5 million people—affected today.
“We don’t know why the numbers are up,” says Peter H.R. Green, director of the Celiac Disease Center at Columbia University. “Gluten just may be more powerful now or there may be other environmental factors.”
Next: “Two weeks later, I was myself. Again.”
Convincing the Skeptics
In terms of evolution, no one was designed to eat gluten. “It’s only in the last 10,000 years, when our ancestors changed their lifestyle from nomadic to settlers who domesticated crops, that gluten came into the picture,” Fasano says. “We don’t have the right enzymes to process it.” But some people don’t seem to be as bothered by the undigested protein.
When friends learn that I’m gluten-intolerant, their first reaction is to remark on how many wonderful foods I must have to forgo. Actually, the sacrifices aren’t that great. I can no longer eat pizza on white or wheat bread, traditional breakfast muffins, many ice creams and candy, and some salad dressings. Dining out requires research, and travel can be challenging, but many Washington restaurants offer special menus, and supermarkets are stocking gluten-free snacks and meals, such as pizza made with a rice-flour crust and pretzels made of gluten-free grains. There’s even a limited selection of gluten-free beers, baked goods, and ice creams that do a good job of satisfying cravings.
Sales of gluten-free foods and beverages in the United States reached $2.6 billion last year. Only 12 percent of those on a gluten-free diet have medical reasons. Others see it as a way to detox, drop pounds, or increase sports performance.
The toughest part for me was figuring out the problem. Because one of my first symptoms was a rash on my buttocks and scalp, my physician, Christine Turner, at the time with Georgetown University Hospital, urged me to see a dermatologist while she ran tests for mononucleosis, Lyme disease, thyroid problems, and a range of other possible culprits.
By the time I met with the dermatologist, the rash had faded and I’d heard the nurse in Dr. Turner’s office relay stories about her own experiences with gluten, so the question about a possible intolerance had been planted. I’d reacted the way most people do: by combing medical Web sites. During my appointment, I brought out a list of gluten-related symptoms, many of which matched mine. Both my dermatologist and her nurse practitioner waved the papers away.
My experience wasn’t unusual. Until recently, gluten sensitivity and celiac disease haven’t been on the radar of most physicians, nor have the topics been given much attention by most medical schools. Of the two, gluten sensitivity has more skeptics.
“If you came to our clinic two years ago and said, ‘Doc, I have these symptoms, and I know that when I eat less gluten I feel better,’ we’d give you a celiac test,” Fasano says. “If it came back negative, we’d tell you to go in peace. If you didn’t eat gluten and thought you felt better, we’d figure it was a placebo effect. That had been our attitude for quite a long time.”
Attitudes are beginning to change, in part due to the BMC Medicine study, which compared blood samples and intestinal biopsies from three groups: 42 subjects with confirmed celiac disease, 26 with suspected gluten sensitivity, and 39 people who served as controls. Those with gluten sensitivity didn’t display the flattened villi or leaky-gut characteristic of celiac, and while their immune systems were triggered, the reactions were less aggressive.
Some experts, such as dietitian Cynthia Kupper, hope the study will emphasize the need for more research on gluten sensitivity, celiac disease, and gluten in general. Kupper—executive director of the Gluten Intolerance Group, a national support organization—maintains that there is concern that gluten may complicate symptoms for some with multiple sclerosis, autism, or schizophrenia: “I think what we’re going to find in the next few years is that this is much bigger than we ever thought.”
Getting Help
I met with Dr. Turner, my physician, after my dermatology appointment. With the exception of low iron levels, all my tests had come back negative. But my symptoms hadn’t subsided. So Turner ordered more tests on my iron levels and reviewed my diet to make sure I was eating enough iron-rich foods. By our next meeting, my iron levels had improved slightly and I was feeling better, almost normal. I told Turner about my gluten research, about my conversation with her nurse, and that for the previous two weeks I’d been avoiding gluten.
Initially, my new diet required a lot of effort. From celiac Web sites, I got lists of troublesome foods and learned to watch for medications and vitamins containing gluten. Then I made my own list and took it to the supermarket so I could consult it while reading labels. I relied on chains such as Whole Foods, which labels most gluten-free products with a green shelf tag. Within a week, I noticed some symptoms had lifted. Within two, I felt like my old self—no more itching, no more headaches, no more fatigue or muscle aches, no more over-the-top anxiety. It felt as though I’d stumbled on a magic bullet.
Turner seemed pleased for me and not at all stunned. She said that more of her patients were insisting gluten was causing problems and that she believed them. Still, she wanted me to undergo a celiac test.
There are no tests for gluten sensitivity, though Fasano’s team is working to identify a biological marker. Meanwhile, people who suspect they have gluten sensitivity are encouraged to undergo celiac testing to rule out that diagnosis. Celiac can be diagnosed with a blood test and an upper gastrointestinal endoscopy in which tissue samples are taken from the small intestine.
I agreed to a blood test but first had to reintroduce gluten into my diet, prompting more symptoms. After ten painful gluten-consuming days, my blood was drawn. The results came back negative, but Turner supported my decision to live gluten-free, saying that the elimination diet seemed to confirm an intolerance. I was relieved and unsure at the same time. I wondered whether I had consumed enough gluten for the test to be accurate. I wondered how I’d explain what seemed like a non-diagnosis to friends and family.
Good Days and Bad Days
Like many who undergo lifestyle-altering diagnoses, I’ve tested mine in the hopes that it might turn out to be only a temporary condition. The last time was about a year and a half ago while in the process of moving. For three weeks, I felt too preoccupied to pay attention to whether my food contained gluten. Bad idea. The major symptom this time was irritability, although I initially associated that with the stress of moving. I also experienced stomach discomfort and dizziness that more than once had me crouching against a wall with my head between my knees.
I eventually consulted a psychiatrist about the irritability, thinking I might need medication. When this doctor learned of my gluten sensitivity, she urged me to eliminate gluten immediately, explaining that in people with an intolerance, eating the protein can cause neurological damage. I replied that gluten couldn’t possibly cause so much tension. On the way home, I indulged in a chocolate biscotti, silently cursing this practitioner with each gluten-laden bite. Then during a moment of clarity, I realized that my combativeness was, well, strange. I resumed gluten-free eating.
Two weeks later, I was myself. Again. I haven’t tested things since. I don’t want to. Life without gluten is a small price to pay for good health and serenity.
Health and feature writer Dana Scarton can be reached via her Web site, danascarton.com.
This article appears in the January 2012 issue of The Washingtonian.