It was the beginning of the summer–school had just ended, camp had not begun. Robin and Stuart Miles-McLean had takentheir two children, Jake and Haley, to the Woodrow Wilson High School pool for family swim night.
At 8:45 on that sultry Washington evening, Haley, a precocious, brown-haired girl who had just finished second grade at Northwest DC's Murch Elementary School, came running up to her parents. Uncharacteristically, she wanted to leave. "We have to go home now," she said.
"Why? We have another 15 minutes," said Stuart, a former professional dancer now with the Environmental Protection Agency. "We just have to go," said Haley. "We have to go."
Haley's insistence led Robin to scan the pool area. Robin's gaze went to the top of the ten-meter diving board, where Jake had been plummeting joyfully into the pool. Now she watched as Jake, apparently changing his mind about the next dive, backed up on the board and began to turn around. As he did, his feet slipped on a wet spot, and he lost his balance. He reached instinctively for the chrome railing but missed. As Robin watched, Jake tumbled off the board and fell headfirst down to its metal-and-tile base, where he lay unconscious and convulsing.
Robin rushed to Jake's side. Blood seeped from his head into the pool gutter. Stuart was quickly at her side. Their immediate thought was that Jake's neck was broken and he shouldn't be moved. At the same time, they were concerned that he might drown in the gutter where his head was.
A man in street clothes approached them. "Who the hell are you?" Robin asked, raising her arms to keep him away. "Don't touch my child."
"I'm an EMT," the man said. "I'm the pool manager." He got a small board and, with the help of Stuart and other adults, maneuvered Jake onto the board to get his head out of the water. He was breathing, but it was labored. An ambulance arrived quickly; it had been passing near the school on its way back from Sibley Hospital, a few miles away. The EMTs picked up the board and took Jake to Georgetown University Medical Center. Stuart rode in the ambulance with his son. Robin drove Haley and some other children home before heading for the hospital.
By the time she arrived, it was clear to doctors that Jake had suffered a traumatic skull fracture and that substantial brain damage was likely. There was bleeding in the front left section of the brain behind the temple. His neck was not broken, and there had been no damage to his spinal column. Except for the skull fracture, Jake had broken no bones.
Dr. Fraser C. Henderson, a neurosurgeon on call at the hospital, leaned over Jake on the operating table. It was 1 AM, some four hours after the accident. For Henderson, a 45-year-old veteran of the Persian Gulf War, it was another night at the office. Ten years earlier he had treated American soldiers aboard a Marine ship; fortunately, there hadn't been many casualties in that war. Returning to the States, he served four years at Bethesda Naval Hospital before moving to Georgetown in 1994.
Henderson had performed thousands of operations like the one he was preparing to do on Jake. From the CT scans, he had a good idea of what he had to do even before he cut into the skull. The brain is so thick with tissue that little can be seen with the naked eye. "What you can actually see," he says, "represents about one half millimeter into the brain."
He cut back the skin over the fracture and gingerly sliced into the skull. What he encountered was discouragingly familiar. Jake had a subdural hematoma and contusion in his left temporal lobe, swelling from which was putting pressure on the brain. He removed blood clots and damaged tissue. It was all he could do. There was bleeding and tissue damage in the basal ganglia and hypothalmic sections of the brain, but those were areas where a surgeon dares not tread. The doctor closed the skull, sewed the ten-year-old back up, washed, and went home.
Jake's survival was in doubt. For 11 days after the surgery, he remained in a coma. On the 12th day, as his mother sat by his side, one eye slid open and then the other. They seemed stationary, transfixed in shock. Nine tubes snaked from medical equipment into various parts of his body. A probe measuring brain pressure stuck out of his head. Jake was not moving. It was the ultimate parents' nightmare.
Robin McLean and Stuart miles had met in a dance class while undergraduates at Indiana University in Bloomington. Robin had grown up in St. Louis, the daughter of an insurance agent; she was studying political science. Stuart, a native of Seattle, was the son of a doctor who had cofounded a group-health cooperative, a radical idea in its time. Stuart had sung in a rock band, then went to study with the Joffrey Ballet in New York City. When his knee gave out, he drove a truck for a while in California and eventually landed in premed at Bloomington. He and Robin were married December 30, 1983, the coldest day on that date in 50 years.
After getting a master's in public administration, Robin got a job at the Environmental Protection Agency in Washington as a regulatory-impact analyst. Stuart was hired at a federally operated fitness center for employees of the Commerce and Justice departments. Eventually he also got a job at EPA as a program administrator. Their first child, Jacob, was born at Alexandria Hospital on January 6, 1989. Haley came along 2H years later, in May 1991.
Robin was a rising star at EPA, a policy wonk with drive and intensity. In 1992 she was transferred to a division office in Ann Arbor, Michigan, and the family moved there. That October, while she was on an assignment in Los Angeles, a motorist rear-ended the rental car she was driving, totalling the car and inflicting a back injury that started a period of constant pain.
Robin's experience with physicians and hospitals had not been pleasant. She felt that doctors didn't understand chronic pain; the ones around her had seemed arrogant. "I knew doctors could be real jerks, and you have to ask a lot of questions," she says.
In 1995, the family returned to Washington and bought a wood-frame home on 39th Street near Connecticut Avenue in Northwest DC. After a year, Robin left the EPA on disability; Stuart remained at the agency.
For grades one through three, Jake attended the neighborhood public school, Murch Elementary. But he was not doing well there. Doctors diagnosed attention deficit disorder and briefly prescribed Ritalin. Still he seemed to have low self-esteem, showed little interest in athletics, and made few close friends. For fourth grade, the family decided to enroll him at Kingsbury Day, a school for children with special needs that occupies several townhouses on Phelps Place near Dupont Circle.
Kingsbury improved Jake's attitude and behavior. Its devoted instructors, rules against teasing, and absolute tolerance of children's "issues" seemed to be doing the job; Jake was beginning to find himself, and his math skills especially were far above grade level.
When his fourth-grade year ended in June 1999, Jake was looking forward to spending part of his summer at an adventure camp and then going on a family trip to Montana. But camp didn't start for a week, and Robin and Stuart were eager to fill the time with activities.
On Thursday, June 17, Stuart and Jake went bicycle riding in Rock Creek Park. On Friday they talked about taking in a Tarzan movie or going swimming. They decided to go swimming.
Two weeks after the surgery, Jake had not improved; on several occasions complications had threatened his life. But his mother, who from the time of the injury had barely left his side, watched every action of the hospital staff and kept a close eye on the brain-pressure monitor to note the effects that various medicines might cause.
Jake was never without a family member nearby. His mother told the nurses firmly that although Jake had suffered brain damage of unknown magnitude, "our expectation is that he will not lose another neuron."
Clashes between Robin and the hospital staff were frequent. Her experience after her own accident had led her to conclude that doctors and nurses sometimes were not candid, frequently were self-protective to the detriment of the patient, and often took steps more for their own convenience than for the patient's betterment.
On one occasion, when Jake appeared to be having an allergic reaction, possibly to a drug, Robin pleaded with the staff to give him Benadryl. Jake had a history of allergies, and Benadryl had been the magic potion. The medical staff resisted, saying Benadryl was too strong for a child in his condition. Eventually, after Jake's tongue and lips swelled, they agreed to give him the Benadryl. The allergic symptoms disappeared.
Robin became such a pain that one doctor called a "family meeting." He said Robin and her parents, who had moved into the Miles-McLeans' house from Missouri, were "taking on too much responsibility" and were "unrealistic about the level of care." He urged the family to abandon its 24-hour-a-day vigil and go home and rest. Robin, he said, was making the nurses "nervous."
Robin exploded, telling the doctor she didn't care if the nurses were nervous or not. Her own experience as a patient had been riddled with episodes of wrong diagnoses and wrong medicines. She wasn't about to risk that in the situation Jake was in.
"One hundred thousand people a year die from medical mistakes," she shouted. "Don't tell me to leave the care of my son alone." The policy analyst knew her numbers–according to research published in November, the figure is 98,000.
Another battle ensued between the family and hospital residents when Stuart insisted that doctors take steps to ward off the possibility of Jake's getting a blood clot in his leg. Stuart worried that if a clot developed in the lower extremities, it could break away, travel to the brain, lungs, or heart, and kill him. He asked that Jake get a TED, a type of elastic stocking, that would ensure an adequate blood flow to his lower extremities. The doctors refused, saying the stocking was for adults, not children. Even after one of Jake's legs began to swell and turn purple, doctors insisted that there was no emergency, that the discoloration was probably the result of medication, not a clot.
Dr. Henderson, the neurosurgeon who had operated on Jake, returned from a trip and came in to see how things were going. He took one look at the leg and called to reserve an operating room. Jake had a serious and fast-moving clot that needed immediate attention. Henderson called in a vascular surgeon, who installed a filter that would keep all clots from traveling toward the brain. For the second time, Fraser Henderson had saved Jake's life.
Doctors at Georgetown still seemed pessimistic about meaningful recovery. For the first two weeks after the accident and operation, Jake moved nothing but one eye. Even his tongue had to be placed back in his mouth when it came out. Every time he was moved for tests, his vital signs would sag. According to his parents, Jake's care was costing Stuart's insurance company, the George Washington University Health Plan, some $1,500 a day. Robin wished she could get him moved to Children's Hospital, but he was not well enough to stand the trip.
Staff neurologists would come into the room and squeeze Jake's fingers and poke his feet, but they saw little evidence of brain function. Still, Stuart and Robin never lost their optimism or hope for a full recovery.
About a week into July, Stuart began responding to some 400 e-mail messages from friends and coworkers. Many were fellow government employees who had loaned him leave time so he could stay as much as possible at the hospital. On July 9, Stuart sent out an update on Jake's condition.
At present, although Jake opened his eyes after 11 days in the coma, he is still in the early stages of recovery from the severe brain injury and the emergency brain surgery he had in the hours immediately following the accident. Although he can't talk, walk, eat, or even sit up on his own, the good news is that all his major physiological systems are working. He is unable to respond reliably to commands. He is now also able to track with his eyes fairly consistently and is just beginning to turn his head to look toward a sound or an object. These little steps add up, and we are encouraged by his strength and courage to continue trying, even when the look on his face tells us that it is very hard and sometimes painful. . . .
Three weeks after the accident, it was clear that Jake could not stay at Georgetown. After much discussion about where he might go, the choice came down to two institutions, a long-term-care facility in Virginia and the Kennedy Krieger Institute in Baltimore. Robin ruled out the Virginia hospital after learning that she would not be allowed to stay in the room with Jake. She worried that he would remain in a semi-vegetative state there, which seemed to be the expectation of many of his Georgetown doctors. At Kennedy Krieger, Robin was told that she could stay in the room. She was determined to not abandon Jake even for a moment. Kennedy Krieger was where he would go.
On July 19, Stuart wrote:
Last week Jake was deemed medically stable and on Thursday, 7/17, he was transferred by ambulance from Georgetown Hospital to Kennedy Krieger Institute in Baltimore. KKI specializes in rehabilitating children with brain and spinal cord problems. Since his arrival at KKI, he has been evaluated by a host of medical experts in order to establish a course of action to carry out his rehabilitation. While Jake is at KKI, Robin is rooming with him and plans to stay there virtually the entire time and I have been driving back and forth on a daily basis taking care of Haley, the dogs, and the house.
Robin felt relieved at KKI. For one thing, doctors there agreed that Benadryl would help Jake sleep and fight off allergies and post-injury muscle spasms; they readily prescribed large doses. They asked Robin what kind of stimuli Jake might respond to. When she told them of his interest in video games, Pokémon, and Nintendo, they ordered a television for the room. Stuart brought videotapes of British comic Mr. Bean, a favorite of Jake's. An even greater change from Georgetown was that the KKI doctors encouraged Robin and Stuart's optimism.
On July 27, Stuart wrote:
Based on their assessments they think Jake will need to be at KKI for at least 10 weeks, and as we move through the weeks they will continuously reevaluate. At the time discharge is deemed appropriate, KKI staff will work with us to arrange ongoing in-home and/or outpatient therapy, as well as identifying and acquiring whatever equipment we may need to care for Jake at home. Although they gave us this initial target discharge date, it is still too early for them to hazard a guess at his prognosis. That uncertainty and ambiguity is hard for us to deal with, but the brain is an incredibly complex organ and since every individual and injury is unique it is not possible for the experts to predict how he will progress. The good news is they are not telling us that our optimism regarding a full recovery is ill-founded, so that is where we have set our sights and that's where we tell Jake he is headed.
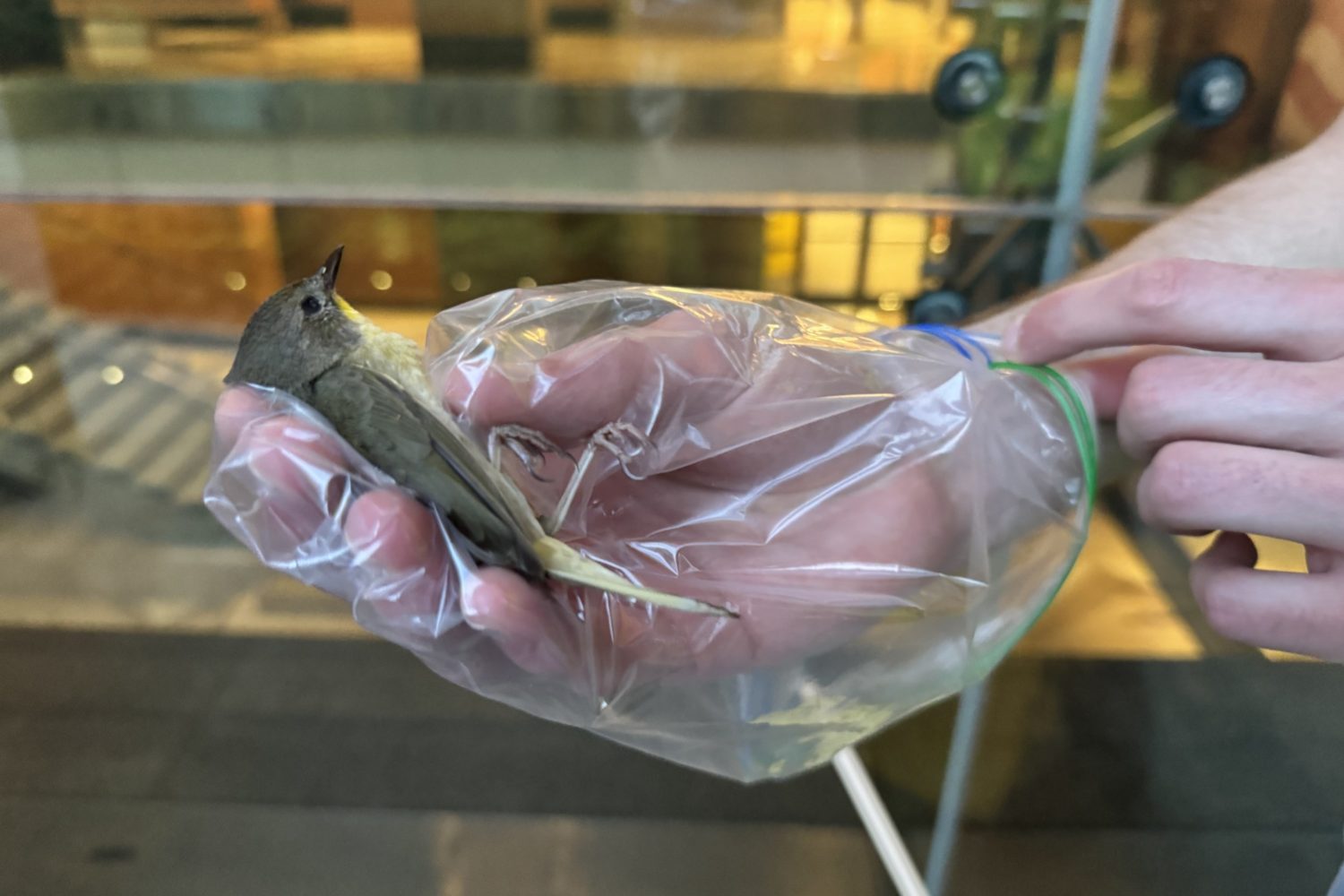
Almost from the moment he arrived at KKI, Jake began to show small signs of improvement. Robin's heart leapt one day when Frances, the family Pomeranian, jumped onto the bed and began licking Jake's face. He moved his arm to pet her.
In the July 27 e-mail, Stuart wrote:
We still see little improvements all the time. . . . Although he can't vocalize because of the tracheostomy, he can smile, open his mouth, and lean back his head in a silent expression of happiness. He was moved to smile on several occasions this week–most notably when his sister sang him a made-up scatological song she composed, which only a 10-year-old boy would appreciate, when his Border terrier puppy Calvin came to visit and licked his face, and when our Pomeranian Frances came to visit and kissed him; and when his Dad put a big goofy ball on his head as though it were a helmet. It was REALLY GREAT to see him smile!
The therapists at KKI were anxious to get Jake out of the supine position. They brought up a wheelchair and began letting him spend time sitting up. His mother began rolling him to physical therapy instead of having the therapists come to his room to touch and rub him. Stuart believed he could feel Jake's trunk and neck muscles getting stronger. By the end of July, Jake was sitting up in the wheelchair six hours a day, with his torso secured so it wouldn't fall to the side. Robin and Stuart noted that he seemed to sleep better at night, presumably because the hours in the wheelchair were tiring him.
On August 12, Stuart wrote:
Jake's progress is agonizingly slow, but the trend is still consistently in the right direction. He continues to improve. On the one side it is difficult to be patient with the slow pace of recuperation and frightening to have no idea how well he will ultimately get. On the other side, the experts tell us that kids with severe brain injuries like his can continue recovering from trauma for up to three years. Accordingly, I try to remind myself periodically to take a deep breath, not panic, and remember that it has been less than two months since he was rushed to the emergency room in an ambulance, bleeding, unconscious, convulsing, and strapped to a backboard.
At 8:30 every morning, Robin began rolling Jake in the wheelchair from therapy session to therapy session. An early task was to get him to lie on his stomach–otherwise, doctors feared, his hip flexor muscles would get so tight that he might not be able to stand up again. In the first week of August he managed to lie on his front for ten seconds–a big success.
In speech and language therapy, experts worked on Jake's facial muscles, critical if he was going to eat or talk on his own. For a long time he had been unable to withdraw his tongue without help. At KKI, he soon was able to relax his jaw enough to allow therapists to work inside his mouth stimulating the muscles for chewing and swallowing. He continued to get food through a tube and to breathe through the tracheostomy tube in his throat. As slow as the progress was, Robin told Stuart, "I think we are seeing more of him every day."
Part of the treatment program at KKI involves the Pets on Wheels program, in which dogs are brought in to help stimulate the children. Stuart had noticed that most of the dogs were large, and some of the children seemed frightened by their size. Frances was nine pounds of lovable fluff. So Robin had Frances certified as a Pet on Wheels, which allowed the little dog to visit all the kids on the floor.
Another breakthrough came in mid-August, when Jake's aunt, Donna McLean, Robin's sister, brought seven pounds of cold spaghetti into the room and proceeded to immerse Jake's bare feet and hands in the noodles. Jake laughed and for the first time moved his limbs voluntarily.
In September, doctors closed the opening in Jake's trachea and allowed him to begin breathing through his mouth and nose. Gradually, mobility returned in his head and neck. Now the speech therapist attached an infrared pointer to a headset with which he was able to "speak" by aiming the beam at sound-producing images on the screen of a computer-like terminal. From his visits with dogs, Jake began regaining voluntary movement in his hands and arms.
By October, Jake was able to lie on his stomach for 30 minutes, could use his facial muscles to take in some food, and had gained more use of his arms and fingers. He was able to play the card game Uno, pinching the cards from a holder with his thumb and forefinger.
Early on, KKI doctors had wanted to implant a permanent stomach tube to replace the nasal-gastro tube through which he had been fed. But Robin resisted the procedure, fearing that if eating were made too easy for him, Jake would lose interest in learning to eat with his mouth again. And if he didn't use his facial muscles for eating, he might not ever use them for speaking. The doctors agreed to hold off, pending studies and tests on whether he would be able to swallow.
Jake was doing so well that the insurance company agreed to pay for four weeks at KKI beyond what had been contemplated. The strength in his legs was returning, and he worked hard at physical-therapy sessions.
On the speech machine, called a Vanguard Communicator, Jake progressed from mastery of 15 icons and sounds to a system of 4,000 words. Using the Vanguard's pictures and letters, Jake was finally able to express himself to his parents and doctors. Many of his cognitive functions had survived the brain injury. His math skills seemed to have disappeared, but his vocabulary was largely intact, as was his memory for facts. He had retained his interest in whales. He could recall most of the important events in his life before the accident, and he was creating new memories. At 8:30 each morning, Jake had "memory group," where psychologists worked on questions about who he was, where he was, and what the day was.
On September 10, Robin e-mailed friends: He has come so far, but has so far to go. We will try to stay focused on the day. They did an MRI of Jake's brain last week and thankfully found nothing new or unexpected. It was sobering, however, to talk to the doctors here that deal with traumatic brain injuries all the time and have them tell us they have no idea what to expect with his progress. They said they rarely see someone with the deep severe injury Jake sustained because most children just don't live through it.
A month later, she wrote:
It is still possible he will talk again, but if he does it will be difficult and hard to understand. I'm just trying to focus on great technology. To his great credit (and my great relief) he is still very outgoing, very positive, and very sociable in a very appropriate way, all things that often disappear after a brain injury. I find myself bouncing between still being extremely sad and grieving over his losses and being grateful for the things that have come back (OK, so sometimes I have to push myself to the grateful spot). Most of the time I focus on the Jake I have, in whom I can see his essential essence, and we make it through another therapy day.
Robin continued to resist the additional feeding tube, and her stubbornness began to pay off. By November, Jake not only was swallowing liquids but had mastered eating chopped and ground foods. He was using the nasal-gastro tube only for water, and his mother pestered the doctors to take that out. Said Robin, "Stuart and I pushed eating so hard that we not only put off surgically implanting a feeding tube into his stomach, they also stopped putting any food through his NG tube."
On October 19, with braces that went from his toes up over his calves, Jake made his way with a walker down the hallway to therapy. When Stuart and Robin asked doctors how well they thought Jake was doing, they were met with shrugs. "I don't know," said one. "We've never seen one make it to this point."
On Halloween, after carving jack-o'-lanterns with Jake at the hospital, Stuart drove his son home to Washington for the night. Stuart dressed Jake in a T-Rex costume, and as Stuart wheeled him from house to house, Jake called out "Trick or treat!" with his communicator device.
On November 18, 1999, doctors gave the okay for Jake to go home for good. Jake's most dramatic progress had been in his ability to move his limbs and to walk. His left hand remained stiff, but he had regained nearly full use of his legs. At the house, he discarded the wheelchair. He was determined to walk, even up and down stairs. But he moved into his sister's room because the stairs to his own room in the attic were too steep.
Wrote Stuart:
Jake was sooooo happy to be home. By the time we got home he was completely off the tube feedings but had to be fed by someone else and the food had to be finely chopped or puréed. In the hospital it was taking an hour for him to eat a meal but at home with all the chaos, some meals were taking as long as two hours for him to consume. He was also very prone to choking, so not just anyone could feed him.
It was an accomplishment when Jake was able to eat his favorite breakfast–a "toad in the hole," a piece of bread with a hole cut out and an egg fried in the center–in less than an hour.
Jake continued to make progress walking. Occasionally he fell. But his balance steadily improved, and he grew stronger and more coordinated. His judgment was excellent, and he wasn't shy about asking for help when he needed it. Jake now used the wheelchair only to hold his 12-pound communicator. Regaining speech continued to be the slowest part of his recovery.
On January 10, Stuart took Jake to the Child's Play toy store on Connecticut Avenue a few blocks from home. After a while, Stuart couldn't tell if Jake wanted to stay or if he was tired. "Do you want to look around some more?" Stuart asked.
Jake put his hands to his lips and said his second word, besides "Mom," since the accident: "Home!"
In mid-February, Jake returned to Kingsbury Day School. There he joins his class for part of the time and spends several hours with a private tutor. His biggest problem at home, say his parents, is trying to argue with his sister without being able to talk as fast as she can. Robin and Stuart had to institute a new family rule for Haley–no argument can be started unless she brings the communicator up the steps for her brother. Failure to provide him an opportunity to respond means she loses the argument by default.
Jake's memory of events before last summer remains intact. He spent a day playing at a friend's house and remembered a CD-ROM game he had left there before the accident. Returning home after playing with another friend, Jake walked inside and headed for the Nintendo game. After a few moments, he remembered something and walked over to his mother, who was sitting at the kitchen table next to the Vanguard. Typing the letters with his right hand–his left is still partially paralyzed–he asked: "Is it time for Dragon Tales?" Assured that he had a few more moments, Jake interjected himself in a discussion of allergies. "I have to wash my hands after I touch a cat," he said. Dogs don't bother him, fortunately, as the family has three. "Frances is my favorite," he says. "She's soft."
When a child suffers a brain injury, says Dr. Henderson, the neurosurgeon, swelling and seizures are common, but Jake has not had those problems. Henderson thinks that much of the damage to Jake's cognitive functions resulted from the twisting and shaking of the brain during the accident. There is no way to know how many axons, or nerve connectors, were severed. But Henderson is an optimist: "Recovery from a brain injury is a four- to five-year process, and over that time he will get a lot back."
Still, the pace of recovery can be grueling for the parents. Robin is frustrated at the loss of Jake's math skills–the former math whiz now struggles to add and subtract. His short-term memory can be erratic: Send him into a room and he might forget what he went for. But not all is for the worse. Although he still suffers from attention deficit disorder, his personality is sweet. "Before the accident," says Robin, "he was moodier, more negative, and had been treated for depression. In some strange ways, he is a happier person, amazingly resilient and much more willing to try things and to work hard."
Says Dr. Henderson, "He will never be the same person that he was, but I think there is a good chance that one day people will meet him and be surprised that he had once had a brain injury."
In one of her last dispatches to friends, Robin wrote:
Over the last two snow days Stuart has worked on getting Jake's [attic] bedroom in order and last night Jake wouldn't go to bed until Stuart finished–he wanted to sleep in his own room. We made a big deal about him walking up the stairs to go to bed–Stuart did the videotaping and Haley provided the color commentary. I hadn't seen Jake this excited since the day he left the hospital. He insisted on setting his alarm clock, getting it tuned to his favorite classical station, and he even spent some time reading "Calvin and Hobbes" in bed before he called me to turn off the light. . . . What a huge step–in October we didn't know if he would ever sleep there again. WOW!