Eric and Jeannie Needle had just found out they’d lost Andrew, their 18-year-old son, when someone came to talk to them about donating his organs. His death was sudden: He’d had a complication from juvenile diabetes and been declared brain-dead.
When the Needles were approached by Dave DeStefano of the Washington Regional Transplant Community in October 2005, they still couldn’t believe their son had died. Andrew was a senior in high school, hoping to get a job as a cook. He had lots of friends—nearly 40 people had come to the hospital. The family had just had its best vacation ever in Rehoboth Beach.
Jeannie knew Andrew wanted to be an organ donor. They’d talked about it two weeks earlier while standing in line at the Motor Vehicle Administration.
“It’s the right thing to do,” he’d said.
But she and her husband weren’t focused on the people Andrew’s organs might help—they were thinking about their son. He looked perfect lying in the hospital bed, as if he were sleeping.
DeStefano sat with the Needles in a room at Washington Adventist Hospital and explained that in order for Andrew to be a donor, doctors would need to keep him on a ventilator for several hours. He asked the Needles what they’d be comfortable donating. Andrew’s heart? His liver? His kidneys?
Eric thought: This isn’t happening.
DeStefano can’t wait until a patient’s loved ones have had time to grieve. About 2 of every 100 deaths can result in organ donation, and most organs are viable for only a short time.
“Sometimes you go home and you’re physically and emotionally exhausted,” says DeStefano, director of recovery services for WRTC. “But you put your head down at night knowing you helped save three, six, seven lives.”
DeStefano, a former paramedic, has had families kick him out of the room. Occasionally he’ll leave and come back. “We need to keep talking with them until we’re comfortable that they understand their choices,” he says. “Too much is at stake.”
Elizabeth Spencer, who spent three years as a recovery coordinator, says she once met with a family who was so hostile after a loved one’s death that the hospital called security. The family eventually agreed to donation.
“You help them understand that there is a face at the end of this,” Spencer says, “a true person with a family like theirs—and they start to realize it’s real.”
Some families tell WRTC coordinators that they shouldn’t be there, because their loved one is going to wake up. In brain death, a patient is on a ventilator, so it appears as though the heart is still beating.
“Very often families are looking for miracles,” says DeStefano, “and they exist in the world of donation—just sadly not for those families. The miracles are going to be someone else’s.”
In 2008, DeStefano and his staff of eight recovery coordinators—most have medical backgrounds—met with 159 families about organ donation. Seventy-five percent agreed to donation. Most patients hadn’t designated themselves donors, so family members were left to decide.
For the Needles, talking to DeStefano was one of the hardest things about that morning in October 2005.
“I can still remember what was running through my mind,” says Eric. “There’s anger. There’s disbelief. It’s something you never forget.”
Kevin Jones got the call around 10 pm, soon after Andrew Needle died. He was at home in bed in Fredericksburg, reading with his wife, Renee.
“This one’s yours,” he remembers the woman from Georgetown University Hospital saying.
“I’ll be there in two hours,” he said.
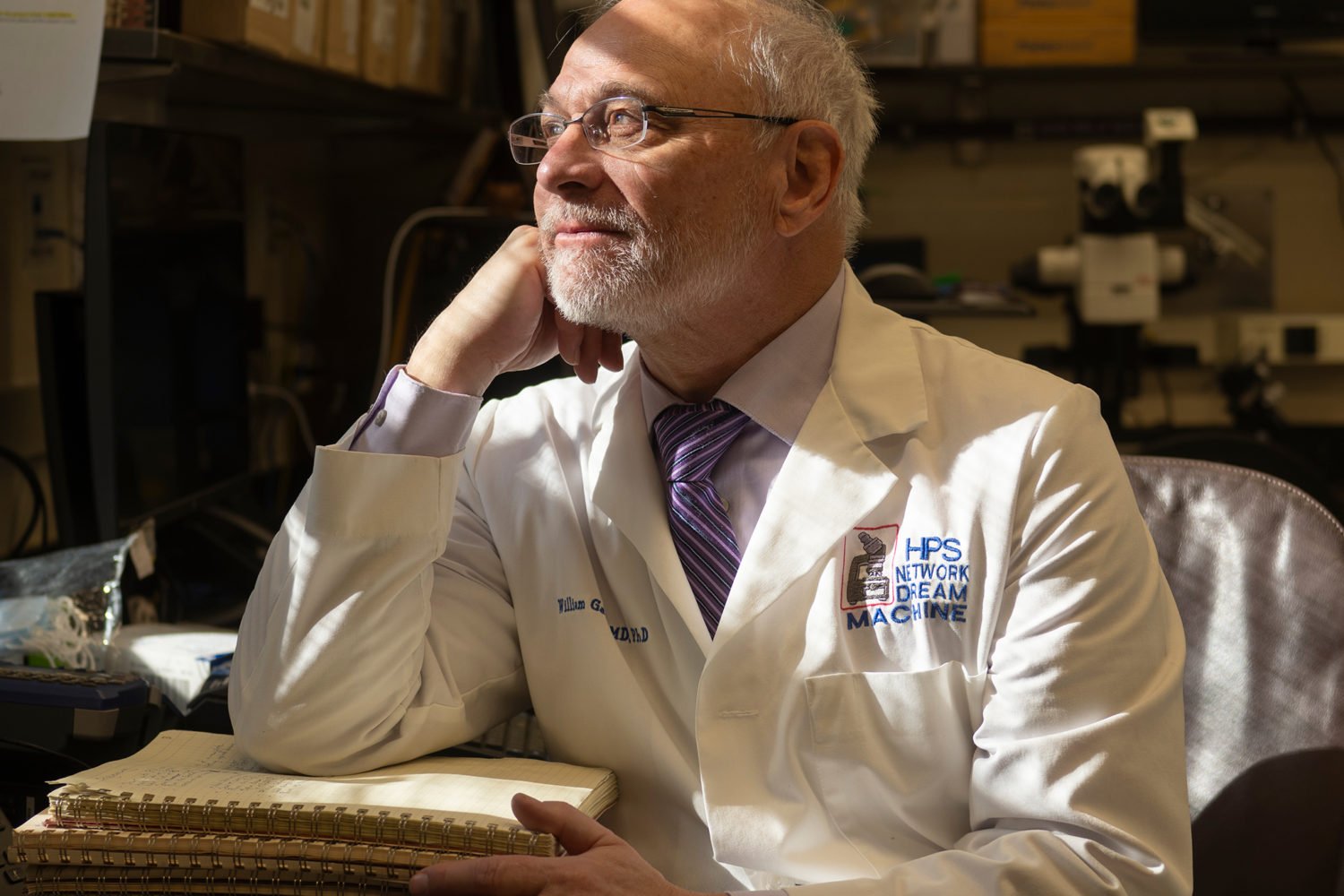
Jones was 52. He’d been diagnosed with hepatitis C four years earlier. The disease, caused by exposure to contaminated blood, can attack the liver for years without symptoms. He’d woken up one morning with what he thought was flu and found out he had end-stage liver disease. Jones, a career Marine, thinks he contracted the virus at a tattoo shop overseas.
Before that night in October 2005, he had been getting his life-insurance forms in order and wondering if he’d see his son graduate from college. A flight of stairs exhausted Jones—sometimes he’d close his office door and lie on the floor. A doctor later said that without a transplant, he wouldn’t have made it past Christmas.
When Jones awoke from his six-hour transplant surgery, he wanted to know whom his liver had come from. Hospitals can’t share donor information, but WRTC can coordinate communication between donor families and recipients if both sides agree. Jones wrote the family a letter.
When the letter arrived at their Silver Spring home a few weeks after Andrew’s funeral service, Eric and Jeannie set it on a table. “We’d read a little bit, and it would sit,” says Jeannie.
Jones talked about his life before the transplant. He told them how thankful he was and asked about their son. If you’re comfortable, he wrote, I’d love to hear from you.
Jones kept writing. The Needles liked getting his letters—they never heard from the two DC men who had received Andrew’s kidneys—but they weren’t ready to write back.
“Once a week we’d say, ‘We really should figure out something to write to Kevin,’ ” says Andrew’s older sister, Kerri. “But how do you sum up Andrew in a letter? You can’t.”
In her first letter two years later, Jeannie started by telling Jones that Andrew had decided on his own to become a donor. The first line of Jones’s response: “Now I know his name.”
When the Needles pulled up to Nicaro restaurant in Silver Spring, where they were meeting Jones for lunch last spring, they considered not getting out of the car. They’d talked to Jones by phone but had never met him.
“There was no hesitation,” says Jeannie. “He just grabbed us.”
His health had been good since the transplant. Recipients are most likely to reject a new organ during the first year; he’d made it almost three. He was training for the US Transplant Games in Pittsburgh, a four-day athletic competition for organ and bone-marrow recipients.
“I remember sitting there for a long time sort of staring at each other,” says Kerri. “I just kept thinking, ‘Andrew is now a part of this man.’ ”
Jones looked at photos of Andrew and noticed his good looks and mischievous smile. The teen had purple hair one week, a Mohawk the next.
“From day one I’ve wondered: What did he look like? How did he sound?” says Jones, who keeps a photo of Andrew on his desk at the Marine Corps base in Quantico. “I started completing the picture.”
He and the Needles talked for three hours. He’d always felt sad for Andrew’s family from a distance, but now there were faces: Why had their son died and he had lived?
This article first appeared in the May 2009 issue of The Washingtonian. For more articles from that issue, click here.